When people first look into ketamine therapy, the first question is usually about dose: How many milligrams, how strong, and how fast it works. That focus makes sense, but it is incomplete. Clinical evidence keeps showing that outcomes depend on the structure around the drug just as much as the amount itself.
The bigger picture matters. Study protocols, monitoring rules, session frequency, and follow-up planning all shape results in real, measurable ways.
This blog looks at what drives success in clinician-guided ketamine treatment, using U.S. trial data and regulatory evidence, so expectations stay grounded and informed.
Quick Answer Summary
Ketamine results are shaped by more than the milligram dose. FDA and VA protocols show that supervised administration, two-hour monitoring, structured induction schedules, maintenance planning, and integration support all influence safety and durability. Trials show that repeated protocols outperform one-off sessions, and continuation strategies reduce relapse risk by nearly half. Ketamine works best as part of a comprehensive plan—including psychotherapy, medication management, and medical oversight—rather than as a stand-alone intervention.
The Treatment Environment: Safety, Setting, and Support
The clinical container is not just a formality. It is part of the intervention itself.
Safety & Monitoring
The FDA prescribing label for SPRAVATO (esketamine), updated in 2025, reports that dissociation occurs in about 61–84 percent of treated patients, while sedation shows up in 48–61 percent. Blood pressure increases appear in 3–19 percent of cases. Because of that risk profile, the label requires supervised administration and at least a two-hour observation window after dosing.
Those numbers come directly from the regulated clinical trial base behind approval. Monitoring is not optional padding. It directly affects whether patients can continue safely and complete a course.
The U.S. Department of Veterans Affairs 2025 ketamine infusion guidance follows the same logic. Their protocol standardizes screening, vitals checks, and infusion procedures. That tells us large health systems treat delivery conditions as outcome variables, not background details.
Therapeutic Setting
When dissociation rates can reach above 60 percent, the setting shapes how tolerable and usable the session becomes. FDA supervision requirements and VA protocol design both assume a controlled medical space. That structure helps patients stay regulated enough to benefit rather than panic or drop out early.
Clinician Expertise
Both the FDA and VA frameworks restrict administration to trained clinical teams. That reflects how altered-state effects need interpretation and containment. Dose alone does not guide someone through that terrain.
Integration: The Bridge Between Medicine and Lasting Change
Acute symptom relief does not automatically convert into lasting functional change. Follow-through matters.
A 2025 U.S. electronic medical record study by Marci and colleagues tracked 163 patients with treatment-resistant depression receiving esketamine. At baseline, 55.8 percent scored in the moderately severe or severe range on PHQ-9. That share dropped to 37.1 percent by the first three months and 25.0 percent by months three to six.
Meanwhile, patients in the minimal-symptom range rose from 5.5 percent to 18.4 percent. Those are multi-month shifts, not instant flips, which suggests that what happens between sessions, including therapy, support, and behavior change, helps lock in gains. The study is observational and used some modeled scores, so it has limits, but the trajectory pattern still matters.
Treatment Frequency & Structure: The Rhythm of Healing
Clinical trials do not test ketamine as a one-off event. They test schedules.
Initial Induction Series
The 2023 U.S. multicenter randomized trial by Anand et al. compared ketamine to ECT in 403 patients with nonpsychotic treatment-resistant depression. The ketamine arm used 0.5 mg/kg infused over 40 minutes, twice weekly for three weeks.
Response meant a 50 percent symptom score drop. 55.4 percent responded with ketamine versus 41.2 percent with ECT. The key point is that the benefit ties to a repeated protocol, not a single exposure.
Maintenance Planning
In the SUSTAIN-1 relapse-prevention trial (Daly et al., 2019), outcomes changed sharply depending on whether patients stayed on esketamine plus an oral antidepressant or switched to placebo with the antidepressant.
Among stable remitters, relapse occurred in 26.7% of those who continued treatment versus 45.3% of those who stopped, with a hazard ratio of 0.49. In stable responders, relapse was 25.8% versus 57.6%, hazard ratio 0.30. Same medication pathway, different continuation plan, and the durability looked very different.
Consistency Over Intensity
FDA maintenance data also shows dosing intervals get adjusted by stability, not pushed high by default. In one label summary, 69 percent of stable remitters received dosing every other week rather than weekly. That pattern favors steady rhythm over brute intensity in ketamine infusion therapy models.
The Comprehensive Care Plan: Ketamine as a Component, Not a Cure-All
Regulatory trials rarely use ketamine alone. FDA esketamine approvals pair it with an oral antidepressant, and relapse-prevention designs keep that background medication in place. That framing positions ketamine therapy for depression as a catalyst within a broader plan.
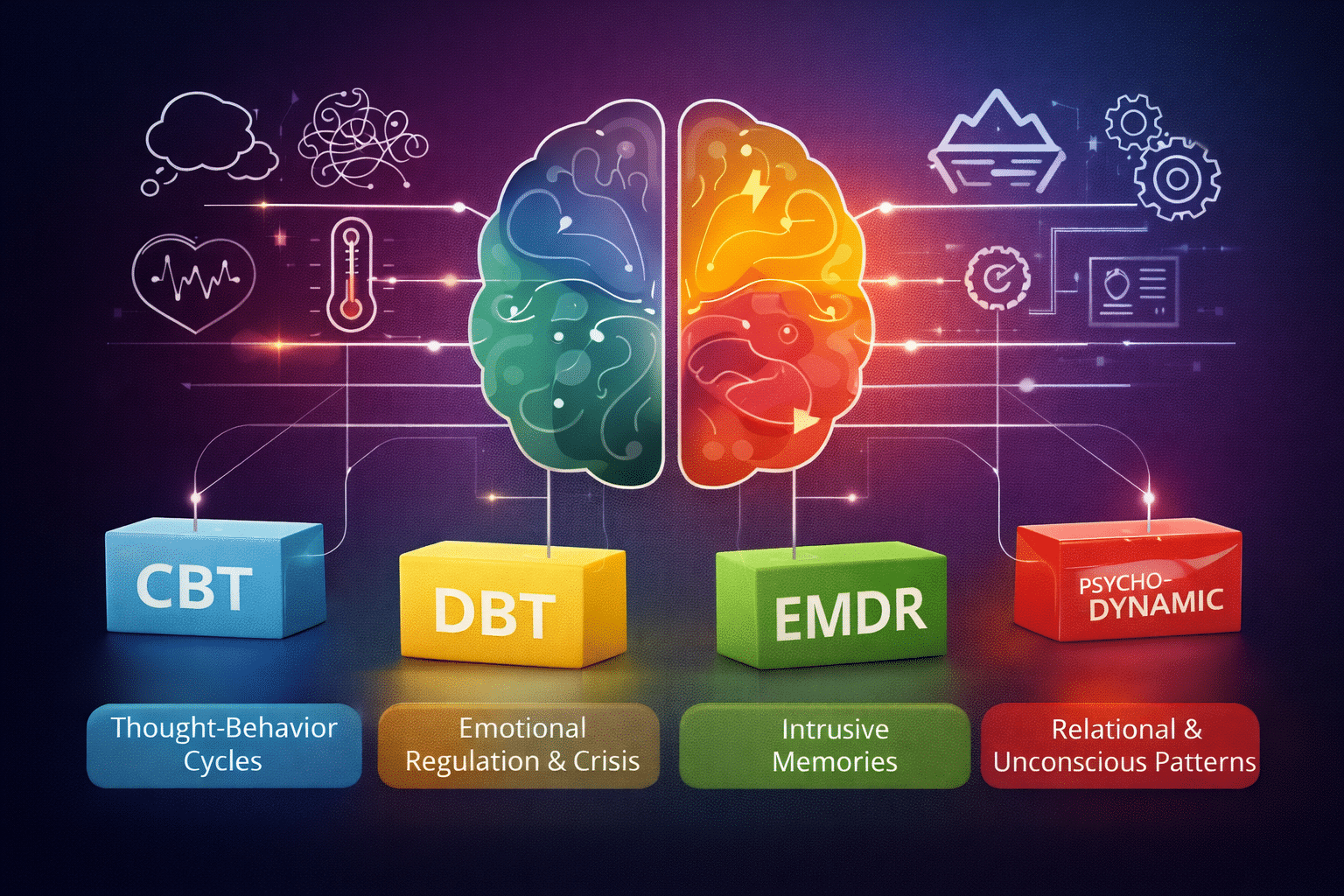
VA guidance places it within treatment-resistant pathways rather than as a standalone fix. In practice, that means psychotherapy, medication management, sleep, and lifestyle supports still carry weight.
Patient-Specific Factors: Biology, Psychology, and Readiness
Individual variation shows up clearly in the data, and it helps explain why responses are uneven across ketamine treatment options.
Neurobiological Baseline
The NEJM ketamine vs. ECT trial focused only on nonpsychotic treatment-resistant depression patients already referred for ECT. That is a very specific clinical subgroup. It tells us the reported response rates apply to that population first, not automatically to every person seeking ketamine therapy for depression in general practice.
Psychological Readiness & Support
VA protocols require formal screening and eligibility checks before ketamine therapy begins. Clinicians assess medical risk, stability, and practical support. That makes readiness part of the treatment decision, not a box-checking exercise.
Co-occurring Conditions
In the Marci et al. EMR study, 64.4 percent of patients had anxiety disorders, and 17.8 percent had hypertension. Those overlaps shift monitoring plans and can influence how someone tolerates and progresses through ketamine treatment.
The Symphony of Success in Ketamine Therapy
Dose is one note. Outcomes come from the whole arrangement: supervision, schedule, continuation planning, and integration. FDA relapse data, VA protocols, and U.S. multicenter trials all point the same way: Structure changes results.
If you are exploring ketamine therapy, look for a program that treats the full ecosystem as part of care. At Zeam in Folsom, Roseville, and Sacramento, we design our ketamine programs around medical oversight, structured frequency, and psychological support, not just numbers on a syringe. Reach out today to talk through options and see what a plan could look like for you.
Key Takeaways
- Monitoring is part of the treatment, not optional padding.
The 2025 FDA SPRAVATO label reports dissociation in 61–84%, sedation in 48–61%, and blood pressure increases in 3–19% of patients, requiring supervised dosing and a minimum two-hour observation window¹. - Large health systems standardize the delivery environment.
The 2025 VA ketamine infusion guidance mandates structured screening, vitals checks, and trained clinical teams, treating setting and procedure as outcome variables². - Improvement unfolds over months, not minutes.
In a U.S. EMR cohort of 163 patients, the proportion with moderately-severe or severe depression fell from 55.8% to 25.0% by months three to six, while minimal-symptom rates rose from **5.5% to 18.4%**³. - Repeated protocols drive response.
A multicenter trial using 0.5 mg/kg twice weekly for three weeks showed 55.4% response with ketamine versus 41.2% with ECT, underscoring that benefits tie to schedule, not a single exposure⁴. - Maintenance planning protects durability.
In the SUSTAIN-1 study, relapse occurred in 26.7% of those who continued esketamine versus 45.3% who stopped (HR 0.49). Among responders, relapse was 25.8% vs 57.6% (HR 0.30)⁵. - Stability guides intensity.
FDA maintenance data show 69% of stable remitters shifted to every-other-week dosing rather than weekly, favoring rhythm over maximum strength¹. - Ketamine is designed as a component, not a cure-all.
Regulatory approvals pair esketamine with an oral antidepressant, positioning it within a broader care plan rather than as a stand-alone fix¹. - Patient factors shape tolerability.
In real-world data, 64.4% had co-occurring anxiety and 17.8% hypertension, influencing monitoring and progression through treatment³. - Integration bridges relief to function.
Multi-month trajectories suggest that therapy, behavior change, and follow-up between sessions help lock in gains³. - Structure changes results.
Across FDA, VA, and multicenter trials, supervision, frequency, and continuation planning consistently predict outcomes more than dose alone¹²⁴⁵.
Citations
- U.S. Food & Drug Administration. SPRAVATO (esketamine) prescribing information, 2025.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2025/211243s016lbl.pdf - U.S. Department of Veterans Affairs. Ketamine infusion for treatment-resistant depression, clinical guidance, 2025.
https://www.va.gov/formularyadvisor/DOC_PDF/CRE_Ketamine_Infusion_for_Treatment_Resistant_Depression_Rev_Oct_2025.pdf - Marci et al., 2025. Real-world esketamine outcomes in U.S. electronic medical records.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12751782/ - Anand et al., 2023. Multicenter randomized trial comparing ketamine and ECT for nonpsychotic TRD.
https://pubmed.ncbi.nlm.nih.gov/37224232/ - Daly et al., 2019 (SUSTAIN-1). Esketamine relapse-prevention trial.
https://watermark02.silverchair.com/jamapsychiatry_daly_2019_oi_190033.pdf