Talk therapy often helps people make sense of what they’re feeling and gradually shift how they handle stress or low mood. Many folks improve, but improvement does not always equal full relief, and that mismatch can leave someone wondering why they still feel stuck despite genuine effort.
Clinicians notice when progress stalls. They watch for patterns showing that talk-based therapy is helping, but not quite getting symptoms to shift. When that happens, they often adjust the plan, maybe adding medical or structured behavioral support to unlock further change.
This kind of shift is not a setback. It is a practical step for people who need more than one approach.
Quick Answer Summary
Talk therapy alone may not be enough when anxiety or depression is severe, persistent, or functionally disabling. Clinical guidelines recommend combined approaches—such as psychotherapy plus medication, structured digital CBT, or collaborative care—when PHQ-9 scores are in the severe range, symptoms have lasted over two years, or progress plateaus. Research shows that higher-structure formats and integrated models can double remission rates and produce meaningful improvements in daily functioning.
When Symptoms Are Severe and Disabling
Severity changes the starting strategy. When symptoms overwhelm daily function, clinicians often widen the plan early so the person can participate in care.
The VA/DoD Major Depressive Disorder Clinical Practice Guideline uses structured measurement tools like the PHQ-9 and defines scores above 20 as severe. In those cases, the guideline suggests combined approaches instead of relying on psychotherapy alone.
The reasoning is practical. Someone with severe depression may struggle to concentrate, process insight, or follow through on skill practice between sessions. Likewise, intense panic or acute suicidal thinking can block engagement with standard therapy exercises.
In those moments, added medical support can lower distress enough to make learning and behavioral change possible. The goal does not change. The path just becomes more supported.
When Brain Chemistry Needs Direct Support
Some presentations of anxiety and depression show strong biological features. Clinicians look for persistent sleep disruption, major appetite or weight shifts, and unrelenting fatigue that does not respond to behavioral tools alone.
The same VA/DoD guideline recommends combined care when depression is persistent for more than two years or when someone has had two or more prior episodes. That pattern points to deeper neurobiological reinforcement. You can think of it like this: Skill-building helps you steer better, but if the engine keeps stalling, you also address the engine.
National data support how common this need is. The 2024 SAMHSA National Survey on Drug Use and Health estimated that 21.4 million U.S. adults experienced a major depressive episode in the prior year, and 64.4% received some form of mental health treatment. Layered depression treatment options are already the norm across the country, not the exception.
How to Recognize a Treatment Plateau
A plateau rarely appears as total nonresponse. More often, insight grows, but emotional and behavioral change lags.
The 2025 psychotherapy outcomes study by Forand and colleagues helps illustrate this. At termination, 79.2% showed meaningful improvement, yet remission reached only 27.7%, and 6.0% showed reliable deterioration. That spread tells clinicians something important. Progress and resolution are not the same thing.
Measurement-guided care helps detect this stall. The VA/DoD guideline recommends repeated symptom scoring over time. When scores flatten across multiple check-ins, clinicians consider adjustments instead of repeating the same plan indefinitely. Options can include medication, modality shifts, or higher-structure programs.
There is also evidence that the structure level matters. A 2025 JAMA Network Open randomized clinical trial of digital CBT for generalized anxiety disorder studied 351 adults and found remission at 10 weeks in 71.0% of the CBT app group versus 34.6% in an online psychoeducation group. At 24 weeks, remission was 77.7% versus 52.0%. That gap shows that changing format and intensity within anxiety treatment options can reopen progress when simpler formats stall.
Functional Impairment That Persists
Clinicians pay attention to how someone feels, but they also watch what those symptoms do to daily life. Struggling at work, drifting away from relationships, or letting basic routines fall apart can say more about the severity of a condition than mood ratings alone. When a person has shown up for therapy consistently yet still cannot manage ordinary tasks, that usually prompts a closer look at what else might help.
Integrated care often changes the trajectory. A 2025 U.S. collaborative care study in primary care followed 148 patients and recorded average drops of 4.8 points on the PHQ-9 and 5.6 on the GAD-7, clear movement in a group that needed more structured support. Those gains came from a model that blended care management, psychiatric input, and steady check-ins.
The point is not replacing talk-based work. It is strengthening it. Sometimes, function improves only when the treatment frame expands enough to match what life demands.
The Case for Integrated Treatment: A Multidimensional Approach
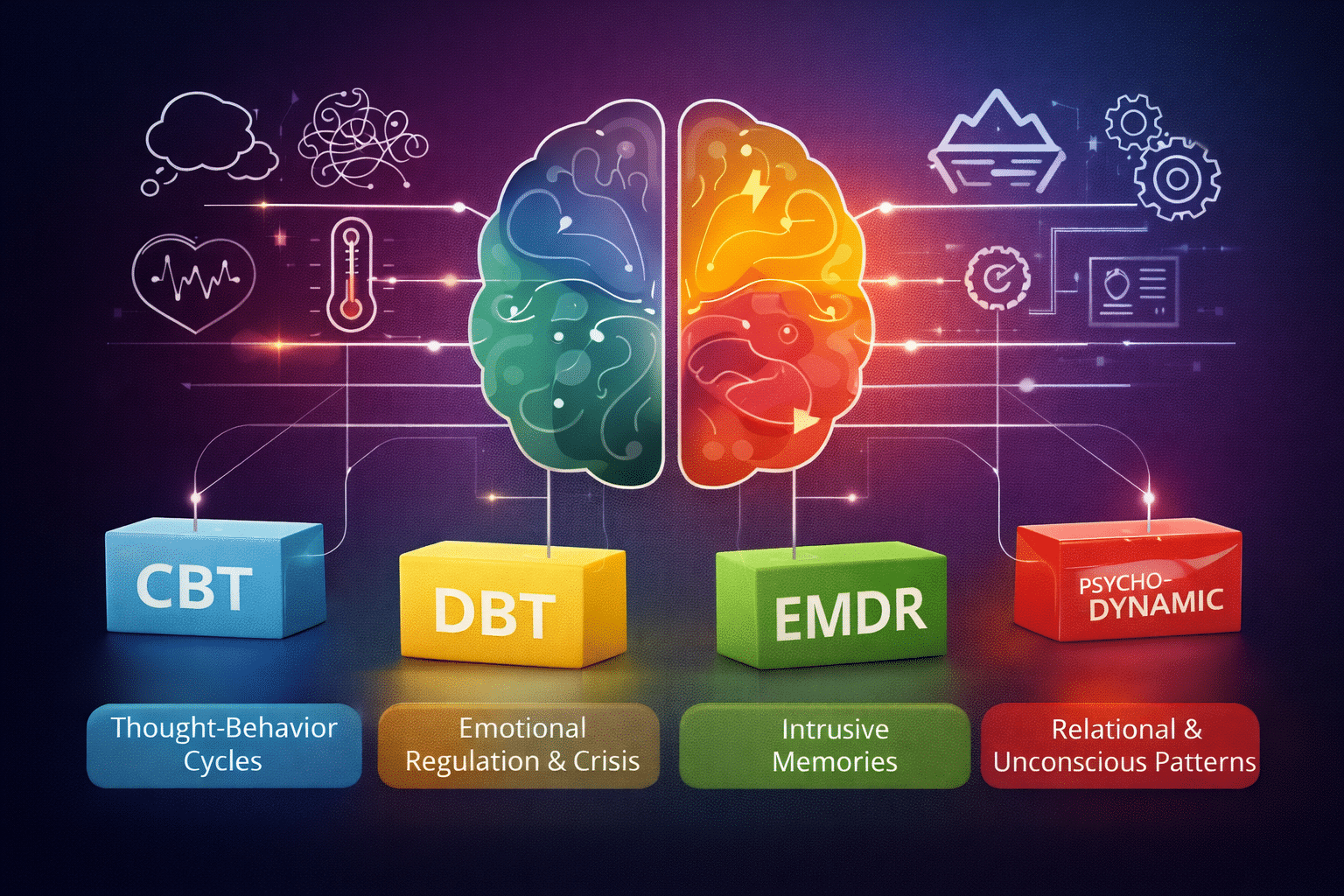
Modern depression treatment and anxiety care often work best when layered. Guidelines and outcome studies point in the same direction: match intensity and modality to need.
The VA/DoD guideline explicitly suggests pharmacotherapy plus psychotherapy for severe, persistent, or recurrent depression. Collaborative care research shows measurable symptom reductions in real clinical settings. The digital CBT trial shows that structured skill delivery can double remission rates compared to lighter educational approaches.
Integrated anxiety treatment plans often combine talk-based skill work with medical support, sleep and activity interventions, and sometimes neuromodulation approaches for resistant cases. The pieces work together. Lower physiological arousal makes cognitive tools easier to apply. Better sleep improves emotional regulation. Structured skill training turns insight into action.
This is collaborative by design. Adjustments happen with the patient, not to the patient.
Evolving Your Path to Wellness
When progress slows, it does not mean therapy has reached its limit. It simply means the plan might need a different mix of support. Many people improve, yet far fewer reach full remission without some kind of adjustment, and noticing that shift shows awareness rather than setback.
Talking through next steps with a therapist or psychiatric provider can help clarify what is getting in the way, especially when symptoms stay intense or daily functioning continues to slip.
At Zeam in Sacramento, Roseville, and Folsom, we design integrated depression treatment options that fit alongside talk-based care, adding support only when it truly helps the broader plan. If you feel stuck or unsure about your next step, reach out to us. We can talk about your situation, go over your options, and help you make a plan for a more stable future.
Key Takeaways
- Severity changes the starting plan.
The VA/DoD guideline defines PHQ-9 scores above 20 as severe and recommends combined treatment rather than psychotherapy alone in these cases¹. - Persistent biology may need direct support.
For depression lasting more than two years or with two or more prior episodes, the same guideline advises layered care to address deeper neurobiological reinforcement¹. - Layered treatment is already the norm.
The 2024 SAMHSA survey estimated 21.4 million U.S. adults had a major depressive episode in the past year, and 64.4% received treatment, reflecting widespread use of multi-modal approaches². - Improvement and remission are not the same.
In a 2025 outcomes study, 79.2% improved, yet only 27.7% reached remission, while 6.0% deteriorated, showing why plans often need adjustment³. - Measurement-based care detects plateaus early.
The VA/DoD guideline recommends repeated symptom scoring over time so clinicians can modify treatment rather than repeating a stalled approach¹. - Higher structure can reopen progress.
A JAMA Network Open trial of digital CBT for generalized anxiety found 71.0% remission at 10 weeks versus 34.6% with psychoeducation; at 24 weeks, **77.7% vs 52.0%**⁴. - Function matters as much as mood scores.
Ongoing difficulty at work, relationships, or daily routines often signals the need to broaden care even when insight is growing. - Collaborative care shows real-world gains.
A 2025 U.S. primary-care program recorded average drops of 4.8 points on PHQ-9 and 5.6 on GAD-7 using integrated management and psychiatric input⁵. - Integrated plans strengthen—not replace—therapy.
Lower physiological distress can make cognitive tools usable, while better sleep and structured skill training convert insight into action. - Adjusting treatment is progress, not failure.
Expanding care reflects clinical awareness and increases the chance of full remission rather than partial relief.
Citations
- VA/DoD Clinical Practice Guideline for Major Depressive Disorder.
https://www.healthquality.va.gov/guidelines/MH/mdd/VADODMDDCPGFinal508.pdf - SAMHSA National Survey on Drug Use and Health, 2024 Annual Report.
https://www.samhsa.gov/data/sites/default/files/reports/rpt56287/2024-nsduh-annual-national-report.pdf - Forand et al., 2025. Psychotherapy outcomes and remission patterns.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12709161/ - JAMA Network Open, 2025. Digital CBT for generalized anxiety disorder randomized trial.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2842818 - 2025 U.S. collaborative care study in primary care.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12706127/