People often consider ketamine therapy only after years of frustration. Traditional antidepressants help many, but for a large group, relief never really sticks.
According to the NIMH, nearly three million Americans live with treatment-resistant depression, and relapse is common even when medications do help for a while. That is usually when someone begins wondering whether ketamine for depression could offer a different path, and whether it is safe to use over time. These are fair questions, especially with so many mixed messages online.
This blog walks through what current research shows, where long-term data are strongest, and how supervised clinical care changes the safety picture in important ways.
Why Ketamine Is Considered for People With Treatment-Resistant Depression
When depression stops responding to standard medications, people often feel stuck. Many have cycled through several antidepressants and therapy approaches with only partial improvement. It becomes exhausting.
This is where ketamine enters the conversation. Research led by NIMH over the past decade showed that a low dose of ketamine, far below what is used in anesthesia, can lift depressive symptoms rapidly for some individuals with treatment-resistant depression. The relief can arrive within hours instead of the weeks traditional medications require.
That speed matters when someone has been struggling for years. But it also raises a different concern: If the effect fades, does that mean someone must use ketamine repeatedly? And if so, what does that mean for long-term safety?
What Short-Term Safety Studies Tell Us About Medically Supervised Ketamine
Short-term data are surprisingly solid, especially for single-dose or early-stage protocols. NIMH researchers pooled results from five clinical trials involving 188 participants, most with severe depression, and looked closely at the side effects that followed a single infusion.
A few patterns stood out. People often described feeling dissociated, spacey, or briefly disconnected from their surroundings, but these sensations almost always peaked within an hour and resolved within two. Nothing in the data suggested worsening memory or decision-making over the next several months.
A small but important detail from this research: Participants were monitored closely. Their blood pressure was checked, clinicians stayed in the room, and someone was always available if the dissociation felt too intense.
That kind of structure explains why these early studies showed no signs of misuse or cravings afterward. It also sets the stage for the real question: What happens when ketamine is used more than once?
The Best Long-Term Data We Have: Multi-Year Esketamine (Spravato) Evidence
Long-term research is harder to collect, but one set of findings offers meaningful reassurance. Esketamine, marketed as Spravato, is a nasal-spray version of ketamine that has gone through the full FDA approval process for ketamine for depression when used with an oral antidepressant. Because of that approval, researchers have been able to follow patients for years, not just weeks.
The largest long-term dataset comes from the SUSTAIN-3 study, which followed more than 1,100 adults receiving intermittent esketamine under clinical supervision. Some participants remained in treatment for over four years, giving researchers an unusually extended view of safety. The overall picture stayed steady.
Side effects like dissociation or dizziness appeared at expected points in dosing sessions but did not intensify over time. Cognitive testing also remained stable, and certain higher-level skills, such as working memory, showed small numerical improvements. Researchers noted a slight slowing in reaction time, though its real-world impact was unclear without a comparison group.
What Risks Still Need Monitoring With Repeated Ketamine Treatment
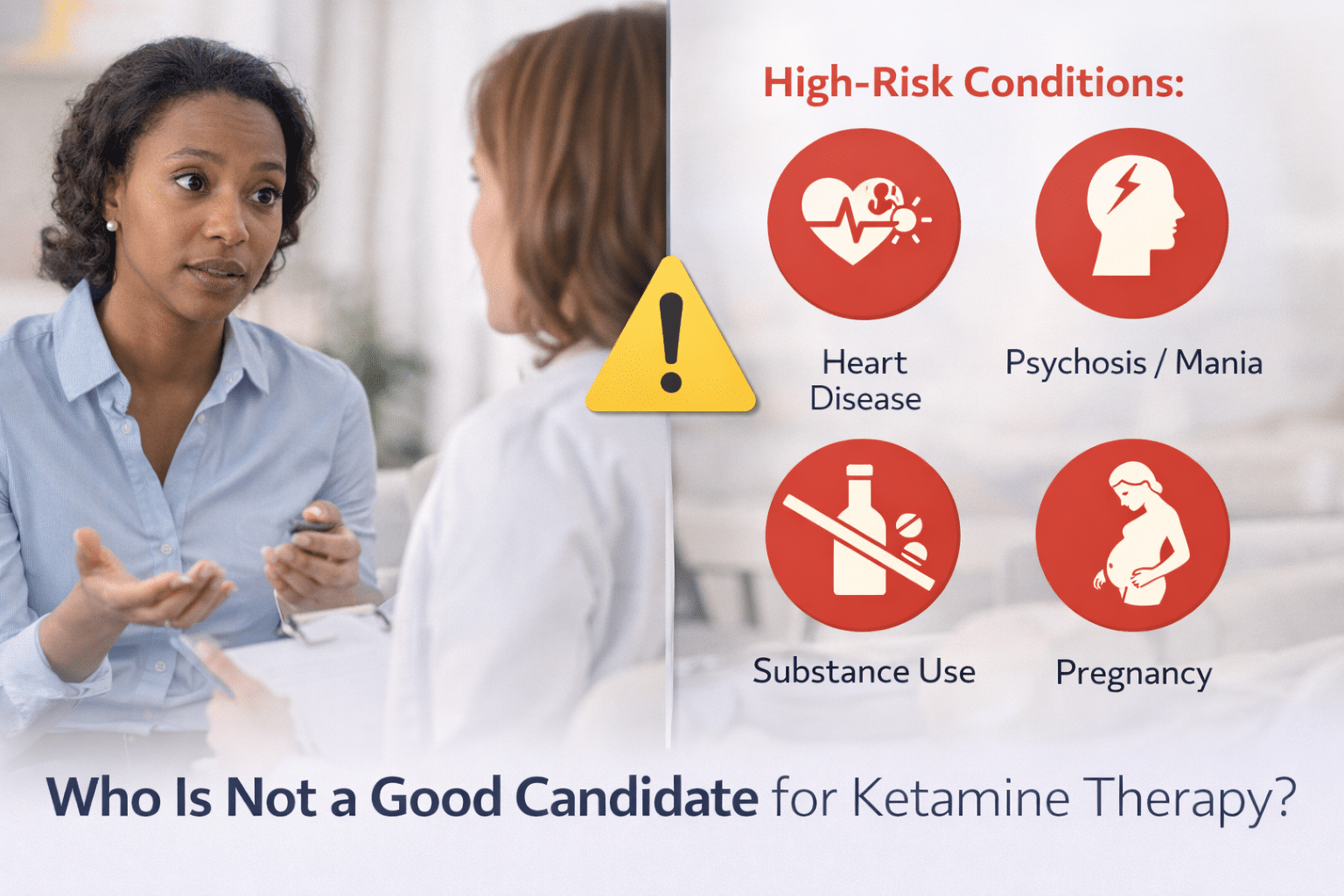
Even with encouraging data, long-term ketamine use is not something to approach casually. Several risk areas need ongoing attention, and this is where honest discussion matters.
Urinary Symptoms
Urinary symptoms are still important to monitor, even though the esketamine study did not show severe bladder damage. Research on recreational use, which usually involves far higher and more frequent doses, shows why clinicians remain cautious. Structured monitoring helps catch early signs of irritation so treatment can be paused or adjusted.
Cardiovascular Effects
Cardiovascular effects also deserve attention. Ketamine can temporarily raise blood pressure, which explains why clinics screen for unmanaged hypertension. Most increases resolve quickly, but repeated exposure means the cardiovascular system experiences repeated stress spikes. Monitoring helps ensure those spikes stay within safe limits.
Abuse and Misuse Risk
Ketamine is a Schedule III substance because it has the potential for misuse. In supervised trials, people did not develop cravings, but the FDA has warned about serious events when compounded ketamine is used at home without medical supervision.
One more thing to acknowledge: We do not yet have decades of data. The longest structured studies reach about six years, which is impressive for a new psychiatric intervention but still a relatively early chapter.
Why Administration Method Matters: Supervised Care vs. At-Home or Recreational Use
The way ketamine is given plays a huge role in determining whether it is safe long-term. The contrast between structured care and unsupervised use could not be sharper.
Spravato, for example, can only be taken in a certified clinic through an FDA risk management program known as REMS. Patients are observed for at least two hours after each dose, vitals are taken, and clinicians make sure dissociation has passed before anyone goes home. This degree of oversight is not optional; it is built into the approval.
Now compare that with compounded ketamine lozenges or nasal sprays delivered to someone’s home. The FDA has been direct about the risks here. Without monitoring, even small shifts in dose can lead to impaired breathing, blood pressure problems, or extreme dissociation. It is not that ketamine suddenly becomes dangerous; it is that the safety net is missing. Recreational use introduces even more variables, from purity to frequency to environmental risk.
When Long-Term Ketamine Therapy Makes Sense, and How Zeam Helps Patients Stay Safe
Long-term ketamine treatment makes the most sense for people who’ve tried several treatments and still feel stuck in patterns of depression that never fully lift. In those situations, the question becomes less about “Is there anything left?” and more about finding a safe, structured way to explore another option. That structure is what keeps long-term use grounded rather than risky.
At Zeam, each person begins with a thoughtful review of their medical and psychiatric history, including heart health, substance use, medication response, and anything else that could shape how their body handles ketamine. Sessions are supervised from start to finish, with clinicians watching for dissociation, blood pressure shifts, or emotional overwhelm.
If you’re considering ketamine and want a medically guided path forward, contact us at Zeam Health & Wellness to start the conversation.
Key Takeaways
- Ketamine is being explored for long-term use mainly for people with treatment-resistant depression, a condition affecting millions each year, because it works through a different mechanism and can act within hours rather than weeks.⁽¹⁾
- Short-term medically supervised ketamine appears safe, with dissociation and blood-pressure changes resolving quickly and no major cognitive decline shown in pooled studies.⁽²⁾
- The strongest long-term data comes from multi-year esketamine (Spravato) studies, where patients were followed for up to 4+ years with stable cognitive performance and no escalating side effects.⁽³⁾
- Certain risks still require monitoring, including urinary symptoms, cardiovascular changes, and abuse potential—especially outside supervised medical settings.⁽²⁾
- The FDA warns against compounded at-home ketamine, citing risks such as extreme dissociation, blood pressure issues, and breathing complications when taken without medical supervision.⁽⁴⁾
- Esketamine (Spravato) is required to be administered only in certified clinics under REMS, highlighting how essential clinical monitoring is for safety.⁽⁵⁾
- Long-term ketamine treatment is safest when given intermittently under structured psychiatric oversight, ensuring benefits while minimizing risks.⁽¹⁾
Citations
- National Institute of Mental Health (NIMH). “Cracking the Ketamine Code.”
https://www.nimh.nih.gov/news/science-updates/2023/cracking-the-ketamine-code - PMC – “The Ketamine Model of Depression.”
https://pmc.ncbi.nlm.nih.gov/articles/PMC8457026/ - Nature — Neuropsychopharmacology, Long-term Esketamine Safety Findings.
https://www.nature.com/articles/s41386-023-01577-5 - FDA Warning About Compounded Ketamine (healthcare provider alert).
https://www.fda.gov/drugs/human-drug-compounding/fda-warns-patients-and-health-care-providers-about-potential-risks-associated-compounded-ketamine - FDA REMS Program for Spravato (Esketamine).
https://www.accessdata.fda.gov/scripts/cder/rems/index.cfm?event=IndvRemsDetails.page&REMS=386