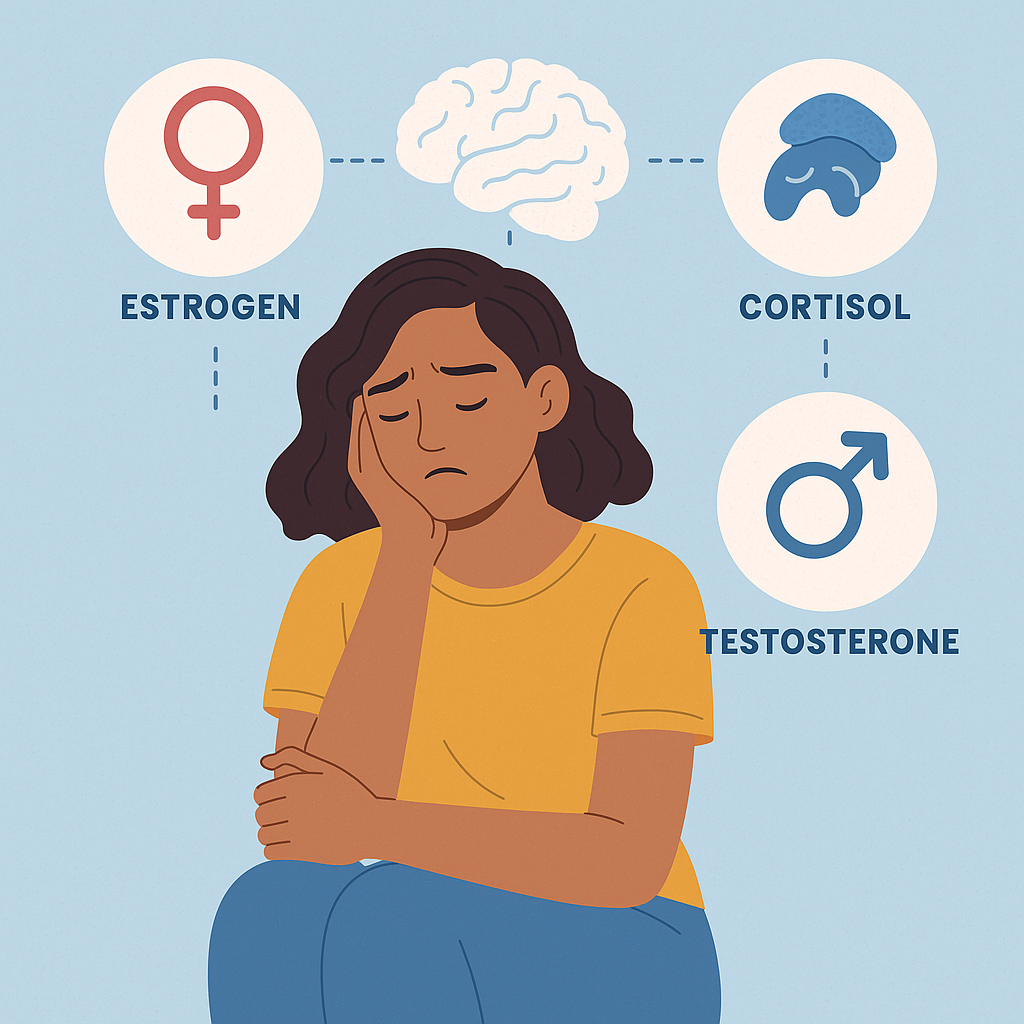
Most people expect hormones to affect their energy levels or sex drive. Fewer realize just how much hormone fluctuations can impact mood, anxiety, and overall emotional stability. When something feels off, such as fatigue that won’t lift, an anxious mind that won’t calm, or sadness that lingers longer than it should, hormones may be part of the story.
Understanding how estrogen, testosterone, cortisol, and thyroid hormones interact with the brain gives us powerful insight into mental health. For many, exploring that connection can lead to better answers and better outcomes than relying on conventional antidepressants or anxiety medications alone.
Here’s what the science shows and why it matters more than ever.
The Hormone-Mental Health Link
Hormones affect brain chemistry in complex ways. They modulate neurotransmitters like serotonin, dopamine, and GABA, all of which influence mood and emotional resilience. When hormone levels fall out of balance, either suddenly or gradually, people may experience symptoms that look and feel like clinical depression or anxiety.
Estrogen, for example, plays a major role in regulating serotonin. It also helps stimulate the release of endorphins and protects nerve cells from damage.
Estrogen increases both serotonin levels and receptor sensitivity. Yet the connection isn’t always linear. Estrogen levels might look “normal” in lab tests, but if the brain isn’t responding to them effectively, symptoms can still occur. That’s one reason some people feel mentally better post-menopause, despite lower estrogen levels.
This same pattern shows up in conditions like premenstrual dysphoric disorder (PMDD), postpartum depression, and perimenopausal mood disruption. These are not isolated problems. Up to 40% of women experience PMS-related emotional symptoms. About 3–9% meet criteria for PMDD. In perimenopause, the risk of a major depressive episode rises two to fivefold, especially during the year after periods stop.
For men, the hormone conversation often centers on testosterone. Although it’s widely known for its role in muscle growth and libido, testosterone also influences emotional regulation, energy, and mental clarity.
A 2021 meta-analysis found that women with depression had significantly different testosterone levels than healthy women. Interestingly, the pattern shifted between premenopausal and postmenopausal groups, highlighting once again how hormone changes (not just deficiencies) may drive mental health changes.
In both men and women, hormone sensitivity and the brain’s response to fluctuations seem to matter as much as the hormone levels themselves.
Anxiety and Fatigue
Chronic anxiety isn’t always psychological. It may reflect deeper biological imbalances, especially in people who also experience brain fog, disrupted sleep, or irritability.
Take cortisol, the body’s primary stress hormone. When the hypothalamic-pituitary-adrenal (HPA) axis misfires, cortisol output becomes irregular. In depression, studies show that this system often loses its feedback control. Some patients produce too much cortisol throughout the day. Others have a flattened rhythm, with cortisol failing to spike in the morning or fall in the evening. These disruptions affect not only energy levels but emotional resilience, memory, and focus.
The HPA axis also communicates with the thyroid and gonadal systems. Disruptions in one often ripple through the others. That means a sluggish thyroid or a poorly regulated menstrual cycle can contribute to physical exhaustion and psychological burnout at the same time.
In a 2022 review, researchers emphasized how fluctuating ovarian hormones increase the risk for depression and anxiety. For instance, they found that over 50% of menstruating individuals with mood disorders experience cyclical symptom flare-ups. These mood shifts can persist even while on antidepressants, a pattern known as premenstrual exacerbation. The underlying issue isn’t always serotonin imbalance. It’s hormonal instability.
Some researchers have even mapped mood changes to specific phases of the menstrual cycle. Estrogen withdrawal during the late luteal phase, for example, can heighten anxiety, worsen irritability, and cause emotional reactivity. Similarly, low-progesterone states can diminish GABAergic activity, making the brain more prone to overactivation and emotional swings.
The result? Symptoms like fatigue, panic, or sadness may have more to do with hormone feedback loops than mental fortitude. If these symptoms persist despite therapy or medication, it’s time to think deeper.
Why Mental Health Alone May Not Be Enough
If you’ve searched for depression treatment near you or tried multiple antidepressants with little relief, you’re not alone. In the STAR*D trial, only one-third of patients achieved full remission after the first antidepressant. Many needed four treatment attempts just to get partial results.
This is where integrated care offers a different path. Hormones don’t operate in isolation. Neither should your treatment.
When mood symptoms persist, it’s worth asking:
- Are there signs of a hormonal pattern?
- Do symptoms spike around cycles, menopause, or stressful periods?
- Are fatigue, irritability, or brain fog part of the picture?
If the answer is yes, working with testosterone replacement therapy doctors near you who understand both psychiatric and hormonal systems can make a dramatic difference. For some, that may mean restoring estrogen or progesterone. For others, it may involve adjusting thyroid levels, addressing testosterone deficiency, or calming the HPA axis through lifestyle and supplements.
The point is that depression and anxiety often have deeper roots than emotions alone. Treating both the mind and the body leads to more complete, enduring recovery.
When to Seek Help and Where to Start
If you suspect your symptoms relate to hormone shifts, don’t wait for things to get worse. The earlier you investigate the connection, the more options you have.
Red flags include:
- Mood swings tied to your cycle, perimenopause, or postpartum period
- Fatigue, low motivation, or sleep problems that persist despite therapy
- Anxiety or irritability that flares before your period or during stressful transitions
- Depression that doesn’t improve with antidepressants alone
At Zeam Health & Wellness, we understand the intimate connection between hormones and mental health. That’s why we offer coordinated services across psychiatry, hormone replacement, primary care, and advanced therapies like TMS, Spravato®, ketamine, neurofeedback, and nutritional psychiatry.
Whether you’re looking for hormone replacement therapy doctors, depression treatment, or anxiety treatment near you, our team provides integrated care that supports your entire well-being. We serve patients in Folsom, Roseville, Sacramento, and through secure telehealth sessions that meet you where you are.
If your symptoms don’t fit into a neat box, that’s okay. We’re here to listen, investigate, and design a treatment plan that addresses the full picture, not just the surface.
Reach out today to take the next step toward balance, clarity, and healing.