People often start treatment expecting one approach to do most of the work. Therapy should carry the weight, or medication should. But real life rarely follows that script. Symptoms ease, then stall, and the person feels caught between “better” and “not quite there.”
Neurofeedback therapy is not a cure-all. It is a way to support the brain’s regulation while the rest of the treatment keeps doing its job. The idea behind adding it is simple enough: If someone already works on their thinking, their habits, or their chemistry, training the brain’s activity patterns might help those efforts land more deeply.
This matters for people exploring neurofeedback for anxiety, because the research leans toward combining approaches rather than expecting one tool to solve everything.
Quick Answer Summary
Neurofeedback therapy is usually added to existing treatment when progress stalls or regulation remains difficult. It helps train the brain toward calmer and more stable activity patterns, which can make therapies like CBT or EMDR more effective and support medication stability. Research shows modest cognitive benefits for ADHD, emerging symptom reductions in depression, and growing use alongside skills-based therapies for anxiety. Clinically, it works best as part of an integrated plan rather than as a standalone treatment.
What Is Neurofeedback and How Does It Work?
Most programs use EEG sensors to monitor the brain in real time. The person sits comfortably while tiny shifts in brainwave patterns change what they see or hear on a screen.
If the brain settles into a smoother pattern, the feedback continues. If it drifts, the feedback pauses. Over many sessions, the brain begins to repeat the patterns it gets “rewarded” for.
It sounds mechanical, but the experience is quiet and uneventful, the kind where a movie brightening or dimming becomes the teacher. Clinics describe this as self-regulation training, something the brain learns through repetition rather than force.
Why Neurofeedback Is Seldom a Standalone Solution
People searching for neurofeedback therapy near them often expect it to stand alone, but the evidence shows it fits better as one part of a broader plan.
In a 2025 meta-analysis, Westwood and colleagues pooled 38 randomized trials (2,472 participants) to test neurofeedback for ADHD. On the primary, probably blinded ratings of total ADHD symptoms, the overall effect was essentially null (SMD 0.04). A clearer signal showed up in processing speed, where performance improved modestly (SMD 0.35).
Helpful, yes, but not a full answer for everyone. So, clinicians often add it cautiously.
This mixed picture also appears across other conditions. Neurofeedback is an approach with uncertain but promising areas. In practice, that means clinicians rarely send someone home saying neurofeedback replaces therapy or medication. Instead, they treat it as an added layer that strengthens the person’s ability to use the tools they already have.
So, how does that integration actually work? Each condition pulls on neurofeedback in its own way.
Enhancing Traditional Psychotherapy
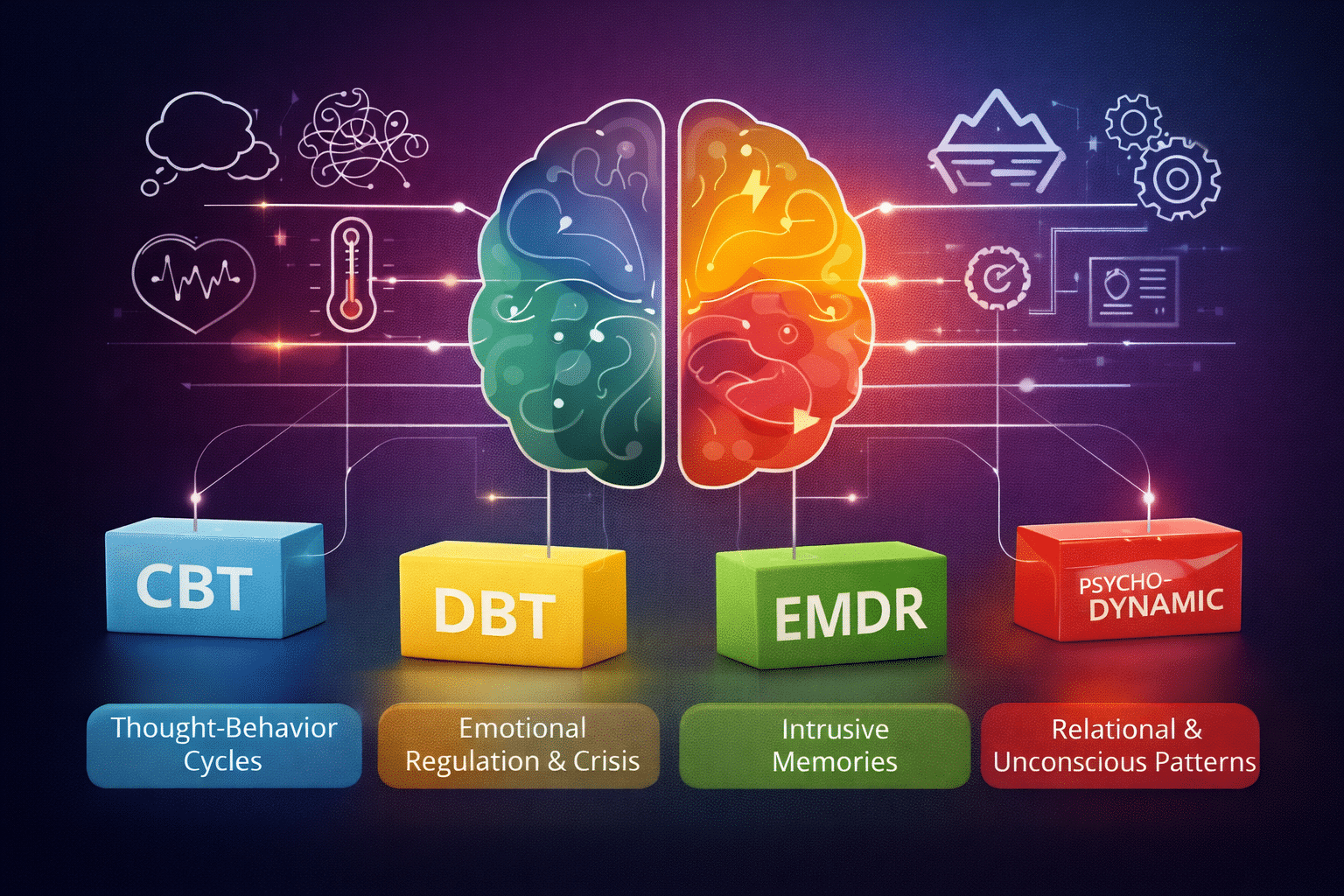
Some people come to therapy ready to learn but unable to settle enough to use the skills. Neurofeedback anxiety protocols often aim to lower that baseline tension, so CBT does not have to fight the body’s alarms.
When the nervous system calms sooner, people have more space to examine their thoughts, and sessions feel less like emotional firefighting. Trauma work benefits from a similar shift.
Hyperarousal can derail EMDR or other trauma-focused treatments; lowering that activation gives the therapy more room to operate. Even mindfulness, which sounds simple on paper, becomes more accessible when the brain has rehearsed calm, steady states during training.
Neurofeedback does not replace the work. It clears some of the clutter that gets in the way.
Neurofeedback for Specific Conditions
For ADHD
The Westwood and colleagues’ findings are unavoidable here because they shape how neurofeedback ADHD protocols are used. With symptom changes so small, providers rarely rely on neurofeedback alone. They combine it with coaching, school strategies, or behavioral therapy.
The processing-speed improvement of 0.35 still matters, though. It suggests neurofeedback gives certain cognitive functions a noticeable lift, which often makes the rest of the treatment plan easier to carry out.
For Anxiety
U.S. researchers continue exploring neurofeedback as part of emotional training. A University of Michigan study protocol describes pairing neurofeedback with cognitive reappraisal practice. The project has not produced results yet, but its design shows the direction anxiety research is moving: Teach the brain to downshift more reliably, then teach the person how to use that downshift in real-life moments. It is a skill-building model, not a symptom-erasing one.
For Depression
The most recent data comes from a secondary analysis of rt-fMRI neurofeedback datasets by Misaki and colleagues. The analysis pooled 95 adults with major depressive disorder (67 active, 28 control) and measured symptoms using MADRS before training and one week after. The active group showed a significant reduction, while the control group did not.
For Comorbid Conditions
People with overlapping symptoms, like anxiety sitting on top of ADHD, often find that neurofeedback does not need to “pick a side.” Because the training focuses on regulation rather than diagnosis, it can support different challenges at once. Still, it remains a piece of the plan rather than the entire strategy.
Working Alongside Medication
Medication and neurofeedback operate in different lanes. Medication shifts chemical pathways. Neurofeedback therapy works on the patterns that those pathways influence.
When the two run together, medication often stabilizes the person enough to fully participate in training, while the training reinforces the stability medication provides. Any medication adjustments stay with the prescriber, but the partnership between approaches is often what makes progress feel steadier.
What to Expect When Adding Neurofeedback to Treatment
The process feels simple from the outside. People sit, watch a screen, and let the feedback guide their brain’s small adjustments. Sessions repeat often because regulation grows slowly, not suddenly.
Most clients describe it as easy to tolerate, mainly because it is non-invasive and does not involve medication. What matters most is consistency. The training builds in layers, so the effects show up the way practice usually does: quietly at first, then more clearly as the person keeps going.
Strengthen Your Treatment Foundation
The real value of adding neurofeedback therapy comes from how it supports everything around it. It helps therapy land with more stability, complements medication rather than competing with it, and gives the brain a repeated chance to practice healthier patterns. Many people feel like their treatment finally works together instead of pulling in different directions.
If you want to know whether this kind of training could support the work you are already doing for anxiety, depression, ADHD, or related concerns, we can help. At Zeam, we build integrated plans that combine evidence-based therapies with approaches like neurofeedback so people experience progress that holds. Reach out to us to schedule a consultation and explore what a more complete path to wellness can look like.
Key Takeaways
- Neurofeedback trains brainwave patterns using real-time EEG feedback to improve self-regulation.
- It is rarely used alone; clinicians add it to therapy or medication when progress plateaus.
- ADHD research shows small symptom change but modest gains in processing speed.
- Depression studies using neurofeedback show promising symptom reductions compared to controls.
- Anxiety protocols increasingly pair neurofeedback with cognitive reappraisal training.
- It supports trauma therapies by lowering baseline hyperarousal.
- Medication and neurofeedback work in parallel, targeting different mechanisms.
- Best results occur with consistent sessions and integrated treatment planning.
Citations
- JAMA Psychiatry: Neurofeedback and major depressive disorder symptom change (secondary analysis of rt-fMRI datasets): https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2827733
- ClinicalTrials.gov protocol: Neurofeedback combined with cognitive reappraisal training for anxiety: https://cdn.clinicaltrials.gov/large-docs/59/NCT06132659/Prot_SAP_000.pdf
- Molecular Psychiatry / Laureate Institute dataset: Neurofeedback effects on depression outcomes:; https://www.laureateinstitute.org/uploads/1/4/1/3/141382282/s41380-024-02880-3.pdf