Most people trying to lose weight focus on the obvious: calorie tracking, exercise routines, and medications like semaglutide. While these all matter, there’s another powerful factor working behind the scenes: sleep.
If you’ve ever stuck to your plan but felt stuck on the scale, this blog is for you. We’re going to unpack how poor sleep can quietly sabotage progress in even the most committed medical weight loss journey. Then we’ll show how the right program can help you take back control.
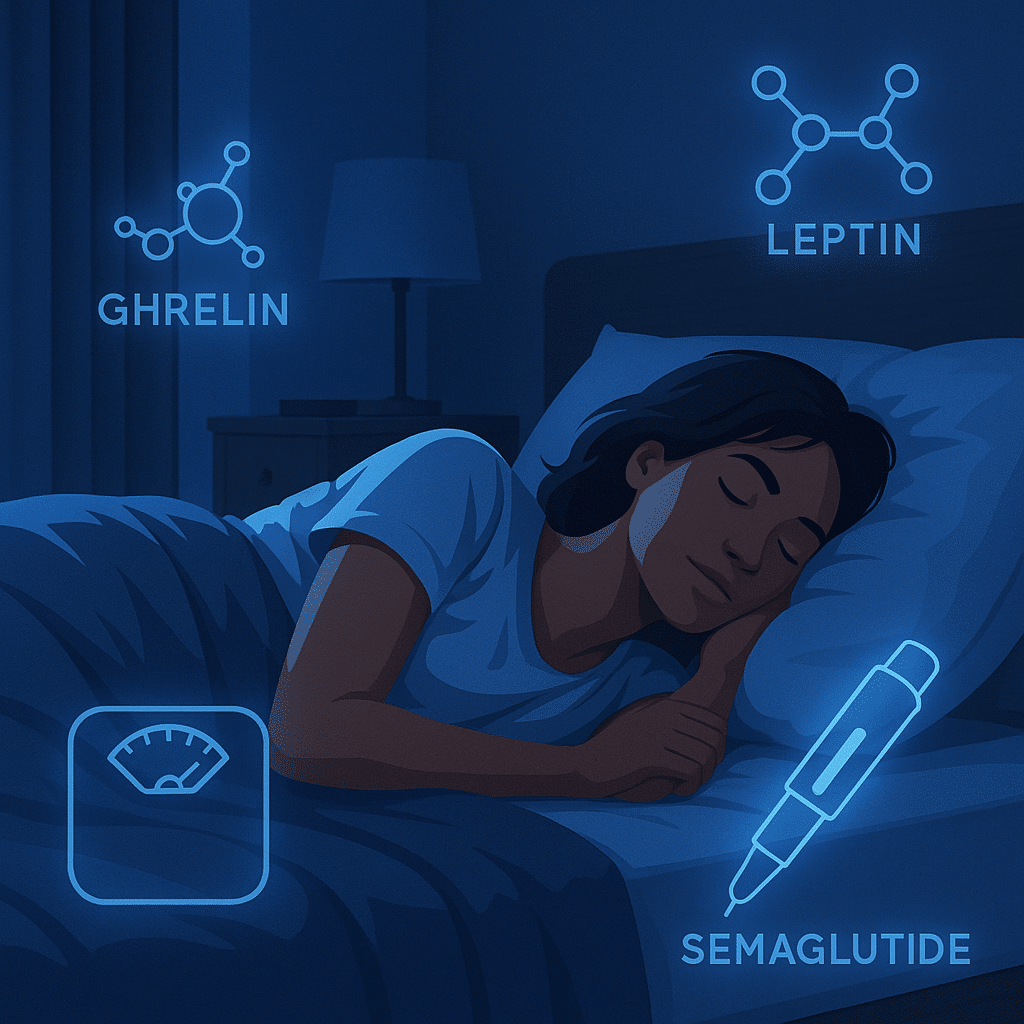
How Sleep Influences Hunger
Sleep isn’t just passive recovery. It actively manages key systems tied to appetite. When sleep is off, even slightly, so are your hunger cues.
Let’s break this down.
The Ghrelin Effect
Ghrelin is sometimes called the “go hormone” because it triggers hunger. Your body ramps up ghrelin when it needs fuel. However, ghrelin can surge even when your body doesn’t need energy, for instance, if you’re underslept.
A 2023 crossover study tracked healthy men after sleep deprivation. Just one sleepless night caused a 17% spike in acylated ghrelin levels, which translated into noticeably higher hunger scores the next morning. The men weren’t more active and didn’t burn more calories. They were simply more likely to eat more because their brains thought they were starving.
The Leptin Drop
Now meet leptin, the “stop hormone.” It signals fullness and helps you stay satisfied after meals. That same crossover study found that sleep loss sharply reduced leptin, leading participants to feel hungrier, even after eating.
When you pair high ghrelin with low leptin, you’ve got cravings, larger portions, more snacking, and a harder time saying no. It’s not about willpower. Your hormones are shouting louder than your logic.
Sleep Loss Impacts More Than Hunger
It would be one thing if sleep only affected appetite. However, it does much more than that, and nearly all of it makes medical weight loss harder.
Cortisol Creep
Lack of sleep puts stress on the body, and with stress comes cortisol. Cortisol isn’t inherently bad. But when levels stay elevated, especially in the evening, fat storage is encouraged, particularly around the abdomen.
According to recent research on circadian rhythms, substantial sleep restriction can raise late afternoon or early evening cortisol levels, even if it doesn’t shift your total 24-hour output.
The pattern might seem small, but it matters. Elevated evening cortisol can subtly signal your body to hold onto fat or feel more alert when you should be winding down. Over time, that throws off the rhythm your metabolism depends on.
Impaired Decision-Making
This one hits home for a lot of patients. You wake up exhausted. You plan to eat clean. But by 8 p.m., your brain feels fried, and suddenly chips sound better than salmon.
What you are experiencing is reduced function in your prefrontal cortex, the part of the brain responsible for willpower and planning. Sleep loss makes that part work more slowly, which leads to impulsive food choices and skipped workouts.
Slowed Recovery
Something that often surprises people is that your body burns calories and builds muscle during sleep. If you’re exercising as part of a medical weight management plan but not getting enough rest, recovery slows down.
In a randomized crossover study of young adults, muscle protein synthesis dropped by 18%, while cortisol levels jumped by 21% and testosterone fell by 24%. Even without any changes to diet or activity, the body shifted into a more catabolic, breakdown-prone state, all from missing a single night of sleep.
Even Semaglutide Works Better When Sleep Is in Sync
There’s no doubt semaglutide helps with weight loss. It reduces appetite, helps you feel full longer, and supports blood sugar control. But even powerful medications don’t work in a vacuum.
If your sleep is irregular, your body still produces high levels of ghrelin and cortisol. That makes it harder for semaglutide to do its job. You’re essentially layering a hunger suppressant over a hormone storm.
One large real-world study out of Japan followed over 350 adults with obesity who were prescribed oral semaglutide. Over the course of treatment, researchers tracked weight loss and sleep habits. Those who improved their sleep, either in quality or consistency, were significantly more likely to respond well to the medication.
Better Sleep for Better Results: What Actually Helps
You don’t need spa-level sleep hygiene. Still, even modest improvements can give your body the reset it needs to support weight loss.
Here are some proven habits to try:
- Stick to a schedule, even on weekends. Consistency helps regulate your body clock and keeps hormonal signals aligned.
- Make your bedroom a true sleep space. That means cool temperatures (around 65°F), blackout curtains, and screen-free wind-down time.
- Cut caffeine by mid-afternoon. Aim for no coffee after 2 p.m.
- Limit alcohol in the evenings. It may help you fall asleep, but it often disrupts deep sleep cycles.
- Build a wind-down ritual. Gentle stretching, low lighting, herbal tea, or journaling. Pick something that signals “bedtime” to your nervous system.
In a randomized trial, adults who typically slept less than 6.5 hours per night were asked to extend their sleep for just two weeks. Consequently, they reduced their daily calorie intake by about 270 kcal, without changing their diet or activity. Energy output stayed the same; it was the extra sleep that nudged their balance in the right direction.
Why Zeam Looks at Sleep as Part of the Weight Loss Puzzle
Most weight loss clinics focus on food, steps, and prescriptions. That’s fine as far as it goes, but it doesn’t go far enough.
At Zeam Health & Wellness, our medical weight loss program was built around the whole person. Our primary care team sees your biology, your schedule, your environment, and your goals, not just your BMI.
When it comes to sleep, here’s what we do:
- Use a questionnaire to screen for sleep apnea risk.
- Offer support for patients struggling with daytime sleepiness, night-shift schedules, or insomnia.
- Coordinate care with specialists if obstructive sleep apnea (OSA) is suspected, especially in patients with obesity or resistant hypertension.
- Incorporate sleep coaching into our broader medical weight management plans, alongside medications like semaglutide or tirzepatide.
If you’re looking for a weight loss clinic near you that looks at the full picture, we’d love to meet you. If you are in Folsom or Roseville, schedule a consultation today, and let’s talk about what’s really holding your progress back and what to do about it.
Key Takeaways
- Sleep affects hunger hormones. Lack of sleep raises ghrelin (hunger hormone) and lowers leptin (satiety hormone), driving cravings and overeating.
- Sleep loss increases cortisol. Elevated evening cortisol levels promote abdominal fat storage and disrupt metabolism.
- Poor sleep impacts brain function and recovery. It weakens decision-making, increases impulsive eating, and reduces muscle repair by lowering protein synthesis.
- Sleep enhances medication results. Patients on semaglutide who improved sleep had stronger weight loss responses compared to those with poor sleep.
- Small improvements matter. Extending nightly sleep by even 1–2 hours reduced daily calorie intake by ~270 kcal in one study.
Citations
- Benedict C, et al. Sleep deprivation and ghrelin/leptin balance. Nutrients. 2023 【PubMed†37537954】
- Medic G, et al. Short- and long-term health consequences of sleep disruption. PMC 【PMC8813037】
- Dattilo M, et al. Sleep and muscle protein synthesis. PMC 【PMC7785053】
- Nishimoto T, et al. Oral semaglutide response and sleep quality. PMC 【PMC12256015】
- Tasali E, et al. Sleep extension and reduced caloric intake. JAMA Intern Med. 2022 【JAMA†2788694】