People tend to start with whatever feels manageable when worry shows up. A few minutes of breathing, maybe a walk, or a late-night meditation video that promises calm.
Those things can help, and they reflect a real attempt to stay grounded. But there is a point where those habits run up against something larger.
In 2024, the National Center for Health Statistics noted that 12.1% of adults reported regular worry or anxiety. That figure hints at how ordinary stress can slide into something steadier. When symptoms begin showing up that often, even well-meant routines start feeling too small.
This guide exists to help people recognize when anxiety treatment at home is no longer enough and when a clinical approach becomes the safer direction.
Quick Answer Summary
At-home anxiety strategies can help early symptoms, but clinical treatment is recommended when anxiety becomes frequent, intense, physically disruptive, or begins to limit work, relationships, and daily functioning. Evidence-based care such as CBT, exposure therapy, medication, and coordinated psychiatric support addresses persistent patterns that self-guided methods cannot reliably resolve.
The Role of At-Home Strategies
Home-based tools make sense as a first layer. They encourage routine, give the mind a place to settle, and create a sense of control. But the relief they offer tends to hover at the surface.
The CDC’s GAD-2 screen was designed to catch patterns that don’t respond to simple changes, and a score of three or more usually signals that a professional evaluation is appropriate. That threshold explains why some people can try everything they know yet still feel pinned down.
But how do you know when the foundation is no longer enough? When does occasional worry cross the line into a condition that requires clinical care?
The following signs are the indicators that professionals use to determine when anxiety treatment needs more than home effort.
Warning Sign #1: Symptoms Escalate in Frequency and Intensity
Anxiety does not always crash in all at once. Sometimes it spreads quietly.
Frequency
What starts as scattered stress can turn into a steady hum that follows you through the week. NHIS data showing widespread regular anxiety captures how easily that shift happens. When the feelings appear most days, it usually means the pattern has taken on a new shape.
Intensity
Panic pressure can rise sharply. Some episodes last longer or show up without warning.
The CDC’s emergency department surveillance recorded 2,338 anxiety-related visits per 100,000 ER visits in December 2025, which suggests how disruptive these spikes can feel when they resemble medical emergencies instead of emotional ones. No amount of anxiety treatment at home can reliably manage sensations that hit this level.
Physical Toll
Tension headaches, stomach swings, or chest tightness can take over daily life. Many individuals arrive in the ER because the sensations resemble medical crises rather than anxiety. When the body becomes the battleground, it’s hard for severe anxiety symptoms to ease with breathing or stretching alone.
Warning Sign #2: When Life Becomes Limited
The internal discomfort eventually shows up in outward patterns.
Work/Academic Decline
Tasks stretch longer than they should. Concentration slips, and deadlines feel heavier. When symptoms start to interfere with everyday functioning, the pattern usually requires more than self-guided management.
Social Withdrawal
Avoiding events or stepping back from friends doesn’t always look dramatic at first. It might show up as uncertainty about going out or leaving early when the discomfort rises. Over time, the social world shrinks, and that isolation deepens the distress.
Daily Functioning
Errands pile up. A simple phone call becomes something to avoid.
A 2026 NHIS-based study of 150,220 U.S. adults reported anxiety or depression symptoms in 68.8% of adults with a general disability versus 40.0% without disability. It did not isolate anxiety disorder alone, but it showed how symptom burden rises as functioning drops.
When errands, calls, or basic routines start feeling impossible, anxiety treatment at home often needs clinical support soon.
Warning Sign #3: The Vicious Cycle of Avoidance
Avoidance works for a moment. That is what makes it tempting. Skip the drive after a frightening episode. Step out of a meeting before your heart jumps again. The brain interprets every avoided moment as proof that the situation was unsafe.
Over weeks or months, the list of avoided places or activities grows longer. Eventually, avoidance becomes the architect of the day. When that happens, the cycle feeds itself, and breaking it usually requires structured intervention rather than continued anxiety treatment in isolation.
Warning Sign #4: Co-Occurring Depression or Physical Symptoms
Anxiety rarely stays in its lane.
Mood Changes
Sadness lingers. People lose interest in things that normally anchor them. Anxiety and depression often show up together, especially for those already struggling with routine tasks.
Sleep Disruption
Nights become restless, and fatigue seeps into everything else. Even strong routines lose their effect when the nervous system never truly resets. That exhaustion can amplify symptom cycles.
Substance Use
Alcohol or other drugs may feel calming for a moment, but they often hide how serious the anxiety has actually become.
The CDC reported more than 49,000 suicide deaths in 2023, along with millions of adults who experienced suicidal thoughts or plans. Any movement toward despair deserves immediate professional support rather than extended anxiety treatment at home.
Warning Sign #5: When You’ve “Tried Everything” and Nothing Helps
People often reach this point quietly. They meditate, exercise, journal, avoid certain foods, and avoid certain people, and still feel overwhelmed.
The NHIS report from 2024 showed that 14.0% of adults received counseling that year, while 5.9% needed it but couldn’t access it due to cost.
Trying “everything” can sometimes mean someone has been fighting without enough support. It’s the condition, not the person, that refuses to budge.
What Professional Anxiety Treatment Provides
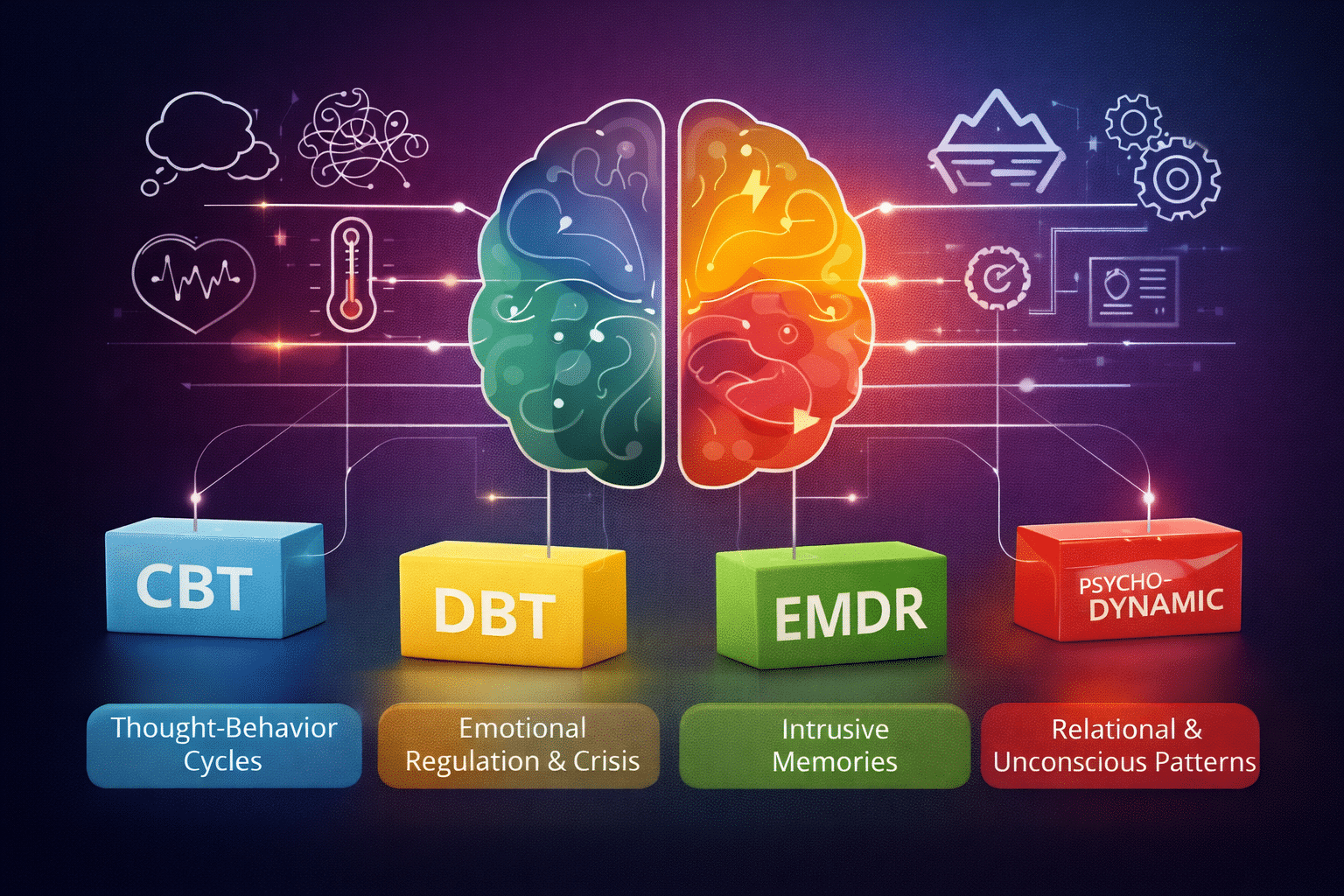
Clinical care brings direction to a confusing experience. Accurate diagnosis helps separate generalized patterns from panic-specific or social-based ones. Evidence-based therapies, like cognitive behavioral therapy (CBT) or exposure work, retrain reactions that keep anxiety alive.
Medication, when appropriate, offers support. And for people approaching crisis, systems like 988 exist for immediate help; SAMHSA reports more than twelve million contacts since the launch, which shows how many individuals rely on that safety net.
The Bridge From Coping to Healing
At-home routines help you steady the day, but they can only go so far once symptoms become persistent or disruptive. Noticing that shift is an important act of self-respect. Effective care exists, and people often improve when they finally receive the support they need.
At Zeam, we guide individuals toward the best treatment for anxiety with therapy, psychiatry, and integrated support designed around their story. If you notice these signs in yourself or someone close, reach out. We can help you move from coping to healing, so schedule an evaluation today and take the next step toward steadier ground.
Key Takeaways
- Regular anxiety affects a significant portion of adults and can progress from occasional worry to persistent symptoms that require clinical care.¹
- Rising intensity, panic-like episodes, and physical symptoms often lead individuals to emergency departments, showing the limits of self-management alone.²
- Functional impairment—declines in work, social engagement, or daily tasks—is a primary clinical indicator for professional treatment.³
- Avoidance behaviors reinforce anxiety over time and typically require structured therapies like CBT and exposure work to reverse.
- Anxiety commonly co-occurs with depression, sleep disruption, and substance use, increasing risk and the need for coordinated care.⁴
- Suicide risk data underscore the importance of early intervention and access to crisis resources such as 988 when symptoms escalate.⁴
- Many adults need counseling but face access barriers, highlighting the importance of timely evaluation and treatment planning.¹
- Clinical care provides diagnosis, evidence-based therapy, medication when appropriate, and integrated support that moves patients from coping to recovery.⁵
Footnotes / Citations
- National Center for Health Statistics. Early Release of Selected Estimates Based on the National Health Interview Survey, 2024–2025.
https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease202506.pdf - CDC. Emergency Department Visits for Mental Health Conditions.
https://www.cdc.gov/mental-health/about-data/emergency-department-visits.html - Peer-reviewed analysis of NHIS data on anxiety/depression and functional impairment in U.S. adults.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12865658/ - CDC. Suicide Data and Statistics.
https://www.cdc.gov/suicide/facts/data.html - SAMHSA. National Guidelines for Behavioral Health Crisis Care (988 and crisis systems).
https://988crisissystemshelp.samhsa.gov/sites/default/files/2025-04/national-guidelines-crisis-care-pep24-01-037.pdf