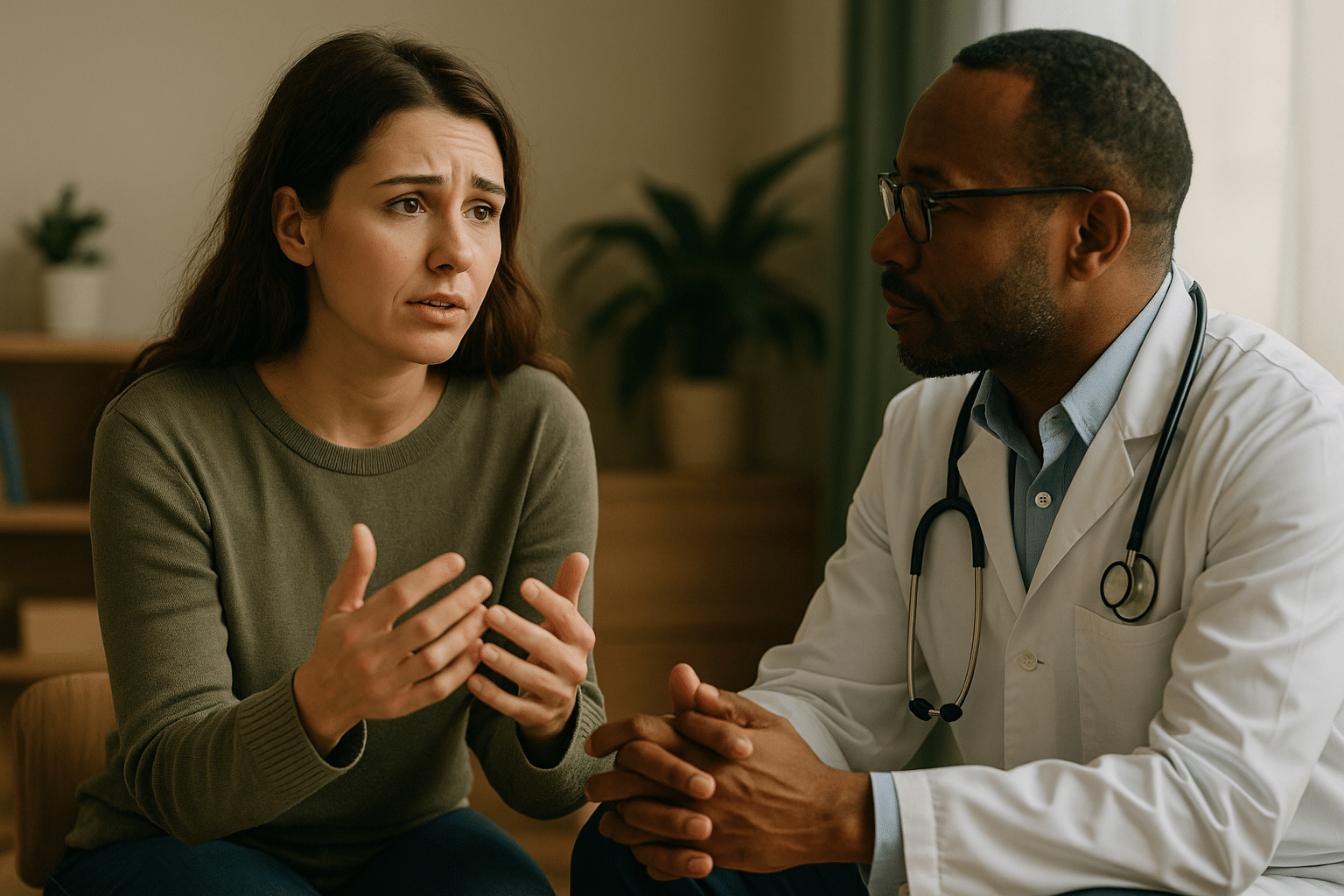
Most people know the feeling: You’re sitting in the exam room, your heart pounding, trying to figure out how to bring up something deeply personal. Your doctor walks in. You have 15 minutes. Do you say it?
Talking about mental health can feel awkward, even with someone trained to help. But your doctor isn’t just there to check your heart or run labs. They’re also your first line of support for mental health concerns. The good news? You don’t have to be perfect. You just must start.
This guide will give you the words, tools, and confidence to begin that conversation, a critical step toward the right depression or anxiety treatment for you.
Why Your Primary Care Doctor Is the Perfect First Step
Your primary care provider knows more than just your blood pressure trends or annual physical history. They also understand how mental health and physical health connect. Changes in mood, energy, or sleep can sometimes signal other conditions like thyroid disorders or vitamin deficiencies. That’s why starting here makes sense. They can rule out physical causes first.
But more importantly, they’re trained to screen for emotional and psychological concerns. The U.S. Preventive Services Task Force recommends routine screening for both depression and anxiety in adults under primary care. These are part of quality primary care services.
Your doctor can also connect you to specialists when needed. That might mean a referral to psychiatry services near you for medication management or recommending therapy services if talk therapy feels like the right next step.
If your symptoms are more complex or have persisted despite prior care, your provider might recommend collaborative treatment, where they work alongside therapists and psychiatric providers. Studies show that this kind of team-based approach can more than double the chances of meaningful recovery.
How to Prepare Before Your Appointment
Feeling prepared makes a huge difference. When you come in with clarity, you give your doctor a better picture, and you’ll feel more in control.
Track Your Symptoms
Start by jotting down how you’ve been feeling over the past two to four weeks.
- Have your sleep patterns changed?
- Has your appetite or motivation shifted?
- Are you more irritable, exhausted, or disconnected?
Even simple notes like “harder to get out of bed” or “trouble focusing at work” can be incredibly helpful.
Write It Down
It’s easy to blank in the moment. Bring a few notes or a short list of what you want to say. This takes the pressure off and ensures nothing important gets lost.
Set an Intention
Decide what outcome you’re hoping for. Maybe you want a referral for therapy services near you, or you’re wondering if medication could help. Perhaps you just want to start tracking your symptoms together. Whatever your goal is, naming it ahead of time helps make the visit more focused and useful.
Simple Conversation Starters (What to Actually Say)
You don’t need the perfect words. You just need something honest and specific. Here are a few options to try:
- The direct approach: “I’ve been struggling with my mood, and I’m concerned it might be depression.”
- The physical symptom lead-in: “I’ve been having trouble sleeping, and I think it’s connected to stress or anxiety.”
- The question framework: “I’ve been feeling anxious for a few months, and it’s starting to affect my relationships. Can we talk about this?”
These are starting points to open the door. According to the National Institute of Mental Health, nearly one in five U.S. adults lives with a mental illness. Consequently, talking about it with your doctor is proactive.
If you’re pregnant, postpartum, or going through hormonal changes, your experience also matters. The American College of Obstetricians and Gynecologists recommends screening for perinatal mood disorders as part of routine women’s mental health care.
You can say:
- “I just had a baby, and I don’t feel like myself. Can we screen for postpartum depression?”
- “I’ve had anxiety before, and I’m worried about how that might show up during pregnancy.”
What to Expect After You Speak Up
When you open up, your doctor’s response should feel supportive, not clinical. They may ask when symptoms started or how often they come up. They might ask how it’s affecting your job, your sleep, your energy.
This is them trying to understand what’s really going on.
They may hand you a short screening tool, like the PHQ-9 for depression or GAD-7 for anxiety. These are brief checklists that help gauge what level of care might be most helpful. Your answers guide the conversation, not define you.
Then, they’ll talk through options. Depending on what’s going on, that could include:
- A recommendation to start therapy, either virtual or in-person
- A conversation about medication
Lifestyle adjustments (exercise, sleep support, nutrition) - A follow-up to check in after a few weeks
If things are more severe, a referral to psychiatry services near you
In some cases, advanced treatments like Transcranial Magnetic Stimulation (TMS) or ketamine treatments like ketamine-assisted therapy may be discussed, especially if other approaches haven’t worked. These are safe, effective options offered for people navigating treatment-resistant depression or chronic anxiety.
Everything you share is confidential. Your provider can’t talk to others about your mental health without your permission unless safety is involved. Therefore, the more you share, the better they can tailor care to you.
You Deserve to Feel Heard and Helped
It’s not easy. Saying “I need help” never really is. But walking into your doctor’s office and naming what you’re feeling is a brave, quiet turning point. That’s the first step forward.
You don’t have to have a breakdown to ask for support. You don’t need a diagnosis in hand. And you don’t need to wait until it gets worse. You can talk about it now. Even if you’re unsure. Even if you’re afraid.
At Zeam Health & Wellness, we work closely with primary care teams in Sacramento, Folsom, and Roseville to make sure mental health support is never out of reach. Whether you’re navigating something new or returning for continued care, we’re here to listen.
Our services include anxiety and depression treatment, as well as care that’s tailored specifically for women at every stage. You don’t have to wait for things to get worse. If you’re thinking about getting help, that’s reason enough. Reach out today.
Key Takeaways
- Your primary care doctor is often the best starting point for discussing mental health concerns like anxiety or depression.
- Bringing notes or a symptom log helps your provider understand your experience and guide care effectively.
- Be open and specific — saying “I’ve been feeling anxious for months” is more helpful than general statements.
- Doctors can use screening tools such as the PHQ-9 or GAD-7 to evaluate depression and anxiety.
- Collaborative care models — where physicians, therapists, and psychiatrists work together — double recovery rates compared to standard care.
- Perinatal and postpartum screenings are essential for women’s mental health, as recommended by the American College of Obstetricians and Gynecologists (ACOG).
- Zeam Health & Wellness partners with local primary care providers in Sacramento, Folsom, and Roseville to ensure mental health support is always within reach.
Citations
- Agency for Healthcare Research and Quality. Collaborative Care Model: An Approach for Integrating Physical and Mental Health Care. AHRQ Integration Academy.
- National Institute of Mental Health. Mental Illness Statistics. NIMH.
- American College of Obstetricians and Gynecologists. Screening and Diagnosis of Mental Health Conditions During Pregnancy and Postpartum. ACOG Clinical Practice Guideline, 2023.