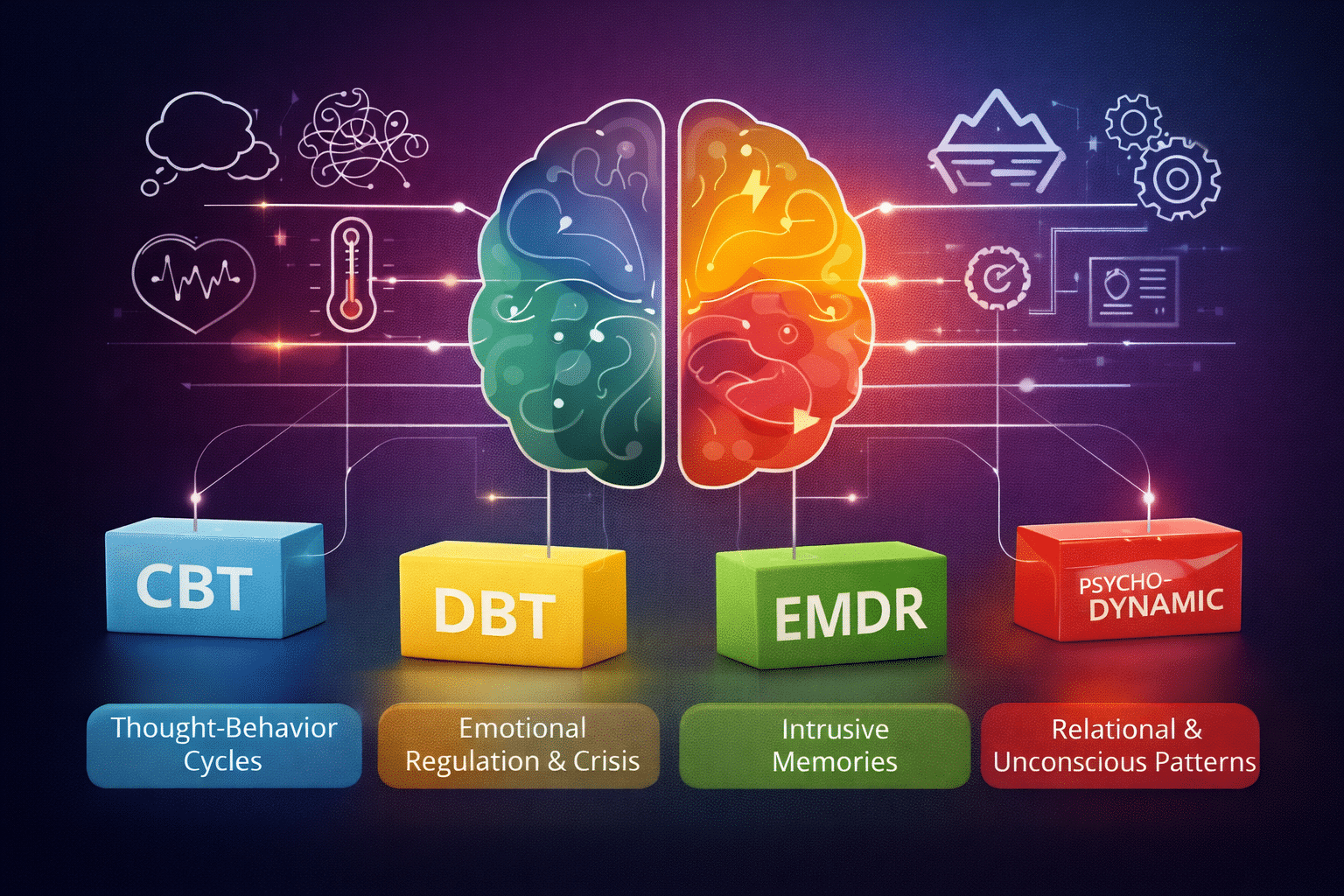
Choosing a type of therapy can feel strangely overwhelming when you first look at the options. CBT, DBT, psychodynamic work, exposure models, and others can sound like competing brands instead of clinical tools. Many people assume clinicians just pick one and see what happens, but that is not how careful mental health care works.
In practice, clinicians follow a structured reasoning process. They study symptom patterns, personal history, and functional impact, then match the mechanism of a specific psychotherapy approach to what is driving distress.
This article breaks down that matching process so it feels more transparent and grounded in evidence.
Quick Answer Summary
Clinicians choose therapy modalities by mapping symptom patterns to treatment mechanisms rather than picking at random. Evidence shows that avoidance-heavy PTSD responds better to Prolonged Exposure, emotional dysregulation to DBT, insomnia within PTSD to CBT-I, and clear thought–behavior loops to CBT with measurement tracking. Assessment, patient preference, and functional impact guide the match, and outcomes improve when progress is measured session by session.
The Initial Map: Conducting a Comprehensive Clinical Assessment
Clinicians start by building a working map of the problem before recommending any therapy approach. That map comes from structured assessment, symptom measurement, and pattern recognition over time.
Symptom Pattern Analysis
Symptom clusters often point toward different treatment mechanisms. Research in PTSD shows this clearly. A 2024 symptom-level analysis by Moshier and colleagues using data from 802 U.S. veterans compared prolonged exposure and cognitive processing therapy.
Prolonged Exposure helped veterans confront reminders more effectively. The reduction in avoidance was strong enough for clinicians to label it a clear advantage over the other therapy. Distress reactions also eased more under this approach, and even hypervigilance, the constant sense of being on guard, shifted in a direction that veterans typically feel in their day-to-day lives.
That matters because clinicians do not just see “PTSD.” They see dominant avoidance, intrusive distress, or belief-based guilt patterns and align trauma therapy methods accordingly. The symptom shape guides the tool choice.
Diagnostic Considerations
Diagnosis still plays a role, but clinicians look inside the diagnosis. A 2024 clinical trial by IsHak and colleagues followed 416 adults with heart failure and depression. Behavioral Activation outperformed usual care, lowering PHQ-9 depression scores by 2.24 points at three months.
The confidence interval stretched from −3.73 to −0.75, which simply means the researchers are highly confident the true effect falls somewhere within that helpful range. Physical and social functioning also improved, showing that people were doing better.
Personal History & Context
Context changes modality choice more than many people realize, and sleep problems offer a good example.
In a 2025 VA randomized trial, Colvonen and colleagues followed 94 veterans with PTSD and insomnia who received Prolonged Exposure alongside either CBT-I or sleep hygiene support. Insomnia improved more when CBT-I was built into the plan.
On the Insomnia Severity Index, the CBT-I plus exposure group moved from 21.26 at baseline to 9.46 after treatment, while the sleep-hygiene plus exposure group shifted from 19.67 to 12.93. Put plainly, both groups slept better, but CBT-I helped people make a bigger jump, with the study also describing a 13.64-point drop versus a 4.61-point drop.
Clinicians often adjust trauma therapy plans when insomnia stays active, because ongoing sleep disruption can keep the system stuck in a higher-alert mode. History and co-occurring symptoms reshape the plan.
Linking Modality Mechanisms to Symptom Profiles
Clinicians think in mechanisms. They ask what keeps the symptoms alive, then select the modality built to interrupt that cycle.
Example 1: CBT for Clear Thought-Behavior Cycles
Some symptom patterns line up neatly with the structure of cognitive and behavioral work, and that is where psychotherapy approaches like CBT tend to land.
In the 2025 Forand study, clinicians tracked PHQ-9 and GAD-7 scores across 18,722 outpatient cases and more than 201,000 sessions. That steady measurement changed outcomes in a noticeable way. PHQ-9 scores dropped an extra 2.4 points, and GAD-7 scores fell 1.6 points more than in settings that did not track progress. The chance of reliable improvement also climbed by roughly 20 percent.
For people whose symptoms follow a recognizable thought-behavior loop, this kind of structured, measurement-guided therapy often fits how the problem actually operates.
Example 2: DBT for Emotional Dysregulation & Crisis
Some situations carry a different kind of urgency. In a 2024 randomized trial, Goldstein and colleagues followed 100 adolescents with bipolar spectrum disorder and recent suicidality. DBT was linked to fewer suicide attempts than standard psychotherapy: Mean attempts were 0.2 versus 1.1 on ALIFE, with incidence rate ratios of 0.32 (ALIFE) and 0.13 (C-SSRS). Clinicians lean toward skills-focused care when safety drives decisions.
Example 3: Psychodynamic/Psychoanalytic for Pervasive Relational Patterns
Some people do not describe one sharp symptom. They describe the same relationship loop playing out again and again. When that pattern drives distress, clinicians may lean toward exploratory psychotherapy that looks at relational templates and enduring emotional themes.
Recent U.S. large RCT data here is thinner than for CBT or DBT, so clinicians rely more on clinical formulation and ongoing response. They use it when attachment and identity themes seem central.
Example 4: EMDR for Trauma-Based Intrusion
Intrusive memories and sensory re-experiencing often point toward memory-processing approaches. Exposure-based and reprocessing models target how traumatic memories get stored and triggered.
That is where EMDR therapy and related trauma-processing methods enter the decision space. PTSD symptom-cluster research, including the 2024 veteran analysis, supports matching intrusion-heavy profiles to memory-focused trauma therapy approaches.
The Role of Client Characteristics and Preferences
Clinical fit is not the only factor. Tolerance and preference matter, too. In the Moshier study for veteran PTSD comparison, completion rates differed: 50 percent for Prolonged Exposure and 61 percent for Cognitive Processing Therapy. That gap suggests that even when two models work, one may feel more sustainable to a given person.
Cognitive style also shapes the decision. Some people prefer structured worksheets and skills. Others respond better to exploratory group therapy conversations or insight-driven dialogue. Clinicians usually present options and explain the reasoning so the client participates in the choice. Buy-in improves adherence, and adherence improves outcomes.
Your Therapy, Precisely Tailored
Effective therapy selection follows a deliberate clinical path. Clinicians study symptom patterns, functional impact, and history, then align the core mechanism of a modality with what maintains distress. Research shows that symptom-level matching, measurement tracking, and targeted adjustments produce better results than one-size-fits-all care.
This process works best as a collaboration. You bring lived experience. We bring assessment structure and modality expertise.
At Zeam, we use comprehensive assessment and careful modality matching, including group therapy and specialized approaches when indicated, to tailor care to each person.
Contact us today to start a focused conversation about your symptoms and begin a personalized path forward.
Key Takeaways
- Therapy choice follows structured assessment, not trial-and-error.
Clinicians build a working map using symptom measures, history, and functional impact before recommending any modality. - PTSD symptom shape guides the method.
In a 2024 analysis of 802 U.S. veterans, Prolonged Exposure produced stronger reductions in avoidance and distress reactions than Cognitive Processing Therapy, helping clinicians align trauma therapy to dominant symptoms¹. - Diagnosis matters, but mechanisms matter more.
Among 416 adults with heart failure and depression, Behavioral Activation lowered PHQ-9 scores by 2.24 points at three months and improved physical and social functioning, showing how mechanism-driven care translates into daily life². - Co-occurring insomnia can redirect the plan.
A VA trial of veterans with PTSD and insomnia found CBT-I plus exposure improved sleep from 21.26 to 9.46 on the ISI versus 19.67 to 12.93 with sleep hygiene, highlighting how sleep symptoms reshape modality choice³. - Measurement-guided CBT improves outcomes.
Across 18,722 outpatient cases and 201,000+ sessions, routine PHQ-9/GAD-7 tracking produced an extra 2.4-point PHQ-9 drop and 1.6-point GAD-7 drop, with about 20% higher chances of reliable improvement⁴. - DBT fits high-risk emotional dysregulation.
In adolescents with bipolar spectrum disorder and recent suicidality, DBT was linked to fewer attempts—mean 0.2 vs 1.1 on ALIFE (IRR 0.32)—steering clinicians toward skills-focused care when safety drives decisions⁵. - Relational patterns may call for psychodynamic work.
When distress centers on repeating interpersonal themes rather than discrete symptoms, exploratory approaches often match the mechanism more closely. - Intrusive memories point to reprocessing models.
EMDR and exposure-based methods target how traumatic memories are stored and triggered, aligning with intrusion-heavy PTSD profiles¹. - Preference influences completion.
In the veteran PTSD comparison, completion was 50% for Prolonged Exposure vs 61% for CPT, showing that fit and tolerability shape real-world success¹. - Collaboration improves adherence.
Presenting options and explaining the rationale increases buy-in, which in turn improves outcomes across modalities.
Citations
- Moshier et al., 2024. Symptom-level comparison of Prolonged Exposure vs Cognitive Processing Therapy in U.S. veterans.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12478573/ - IsHak et al., 2024. Behavioral Activation for depression in adults with heart failure, randomized trial.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2814018 - Colvonen et al., 2025. CBT-I combined with exposure for PTSD and insomnia in veterans.
https://www.ptsd.va.gov/professional/articles/article-pdf/id1649937.pdf - Forand et al., 2025. Measurement-based CBT outcomes across large outpatient sample.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12698511/ - Goldstein et al., 2024. DBT for adolescents with bipolar spectrum disorder and suicidality.
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2809647