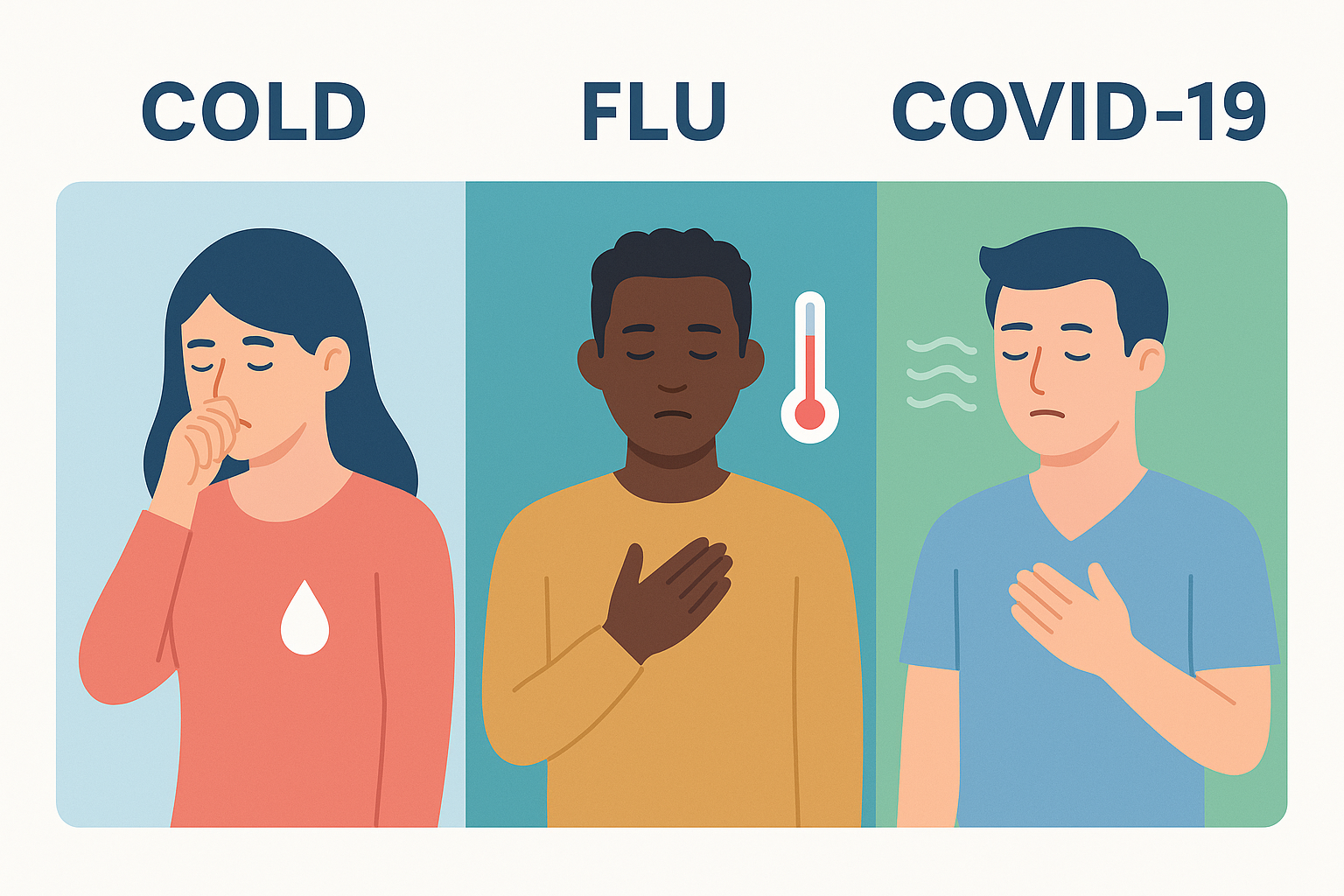
Every fall, the same question comes back: Is this runny nose or cough just a cold, or could it be something bigger? The overlap of symptoms fuels anxiety. People want to know if they are facing a cold, flu, or COVID situation, or simply dealing with seasonal sniffles.
This guide looks at cold vs. flu vs. COVID: the differences, similarities, and red flags that require medical attention. While it is often difficult to self-diagnose based on symptoms, there are cues, time frames, and testing options that can assist. The main point is that knowing when to seek care can help relieve some anxiety this season.
Symptom Snapshot: A Quick-Reference Table
Symptoms often blur together, but comparing them side-by-side gives clarity.
| Symptom | Common Cold | Flu (Influenza) | COVID-19 |
|---|---|---|---|
| Fever | Rare or mild | Common, sudden, often high | Common, varies by case |
| Cough | Mild to moderate | Dry, persistent | Dry or productive |
| Shortness of Breath | Rare | Rare | More likely, especially with moderate cases |
| Fatigue | Mild, short-lived | Sudden, severe | Variable, sometimes prolonged |
| Body Aches | Mild | Pronounced, whole-body | Possible, less predictable |
| Sore Throat | Common | Sometimes | Common |
| Runny Nose | Very common | Less common | Possible |
| Sneezing | Frequent | Rare | Rare |
| Loss of Taste/Smell | Rare | Rare | Still occurs, but less universal now |
| Symptom Onset | Gradual | Abrupt, within hours | Variable, can take 2–14 days |
This table is not a diagnosis tool, but it captures the broad strokes that doctors notice when comparing flu vs. COVID-19 symptoms in 2025, alongside colds.
The Common Cold
Colds are still the most frequent upper respiratory infection in the fall. They creep in slowly, usually starting with a scratchy throat or a few sneezes. A runny or stuffy nose becomes the main complaint. Unlike flu or COVID, colds rarely bring high fever or full-body aches.
Most colds improve within 7 to 10 days, though the cough and congestion may linger for another week. Children often have longer colds than adults. A typical cold feels more annoying than alarming. Rest, fluids, and over-the-counter medicines usually do the job. Antibiotics are not helpful since viruses, not bacteria, cause colds.
Influenza (The Flu)
Flu season usually begins in October and peaks in winter. Unlike the cold, the flu often feels like it hits out of nowhere. Someone can feel fine in the morning and miserable by evening. The abrupt onset of high fever, chills, severe fatigue, and pronounced muscle aches sets it apart.
The flu is very contagious and can be severe, especially in individuals 65 years of age and older, pregnant women, and people with chronic health conditions. Sometimes, people are hospitalized or have complications like pneumonia.
The average incubation period for the flu is about two days. As a result, people can spread the flu to others before they have any idea they are ill.
Treatment matters. Prescription antivirals like oseltamivir work best if taken within 48 hours of the first symptoms. That short window makes early recognition critical. If you fall into a high-risk category, do not wait for lab confirmation to reach out to a healthcare provider.
COVID-19
COVID-19 still shows up every fall, though the way it looks keeps shifting as new variants circulate. For many people, the illness feels almost identical to the flu.
Fever, cough, sore throat, congestion, and fatigue are the most common complaints. Some patients continue to experience loss of taste or smell, but that hallmark symptom has become less frequent than it was in 2020 and 2021.
One detail that sets COVID apart is the chance of shortness of breath and exhaustion that lingers for days or weeks. Research also shows the incubation period can stretch anywhere from two to fourteen days, with most cases emerging around day four or five. That longer infectious window is one reason outbreaks can spread quickly through homes, classrooms, and workplaces.
Because cold symptoms vs. COVID-19 symptoms overlap so much, testing remains the best way to know what you are dealing with. A single negative rapid test is not enough. Experts recommend retesting within 48 hours or confirming with PCR, especially if antiviral treatment may be an option.
When to See a Doctor
The question many people ask is when to see a doctor for the flu or COVID. Most mild colds can be managed at home, but there are situations where professional care is essential:
- Difficulty breathing or persistent chest pain.
- High fever that does not improve with over-the-counter medicine.
- Confusion, disorientation, or inability to stay awake.
- Worsening of chronic conditions such as asthma, diabetes, or heart disease.
- Symptoms that improve but then return stronger.
High-risk groups should not wait. Older adults, pregnant people, and those with compromised immune systems need to call as soon as a fever or cough begins. Quick action can open the door for antivirals that prevent serious outcomes.
Why Testing Is the Only Sure Way to Know
Because flu and COVID-19 symptoms are almost identical, self-diagnosis is unreliable. Cold patterns are easier to guess, but even they can overlap. That is why testing remains central to care.
COVID antigen tests work best a few days into symptoms, but a first negative is not always the last word. Retesting in 48 hours or confirming with PCR adds accuracy. Flu tests can confirm influenza, but in practice, many doctors start treatment without waiting for results if a patient is high-risk and the community spread is high.
Stay Informed, Not Anxious
It is easy to get lost when every cough or sneeze feels like a warning sign. Colds, flu, and COVID share so much that guessing often creates more stress than answers. A cold usually hangs around the nose with sneezing and congestion. The flu shows up fast, with fever and sore muscles that knock you down. COVID is the wild card, sometimes looking harmless and other times hitting much harder.
Instead of worrying, watch how symptoms unfold. Did they start suddenly, or creep in? Is the fever stubborn, or is breathing harder than usual? Those details, plus a test, can point you in the right direction. Severe or lingering issues always deserve medical attention.
If you are uncertain whether you are dealing with a cold, the flu, or COVID-19, do not wait it out in doubt. Contact Zeam Health & Wellness. We offer preventative care services in Roseville and Folsom.
Key Takeaways
- Symptom overlap creates confusion: Colds, flu, and COVID-19 often look similar, but symptom onset speed and severity provide helpful clues【https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-vs-flu/art-20490339】
- The flu hits harder and faster: High fever, body aches, and sudden fatigue distinguish influenza, which often requires prompt antiviral treatment within 48 hours【https://www.cdc.gov/flu/hcp/antivirals/summary-clinicians.html】
- COVID has the widest range: Shortness of breath, longer incubation (2–14 days), and lingering fatigue or “long COVID” symptoms remain distinguishing factors【https://www.cdc.gov/mmwr/volumes/73/wr/mm7316a2.htm】
- Colds stay mild: Gradual onset, runny nose, and sneezing are common, but severe fever and body aches are rare.
- Testing is essential: Because symptoms overlap, testing (antigen or PCR for COVID, flu swabs) remains the only way to confirm infection and guide treatment.
- Seek care for red flags: Trouble breathing, persistent fever, confusion, or worsening chronic conditions warrant immediate medical evaluation.