Some people feel anxiety in their chest, while others carry it in their gut. If that sounds familiar, you’re not imagining things.
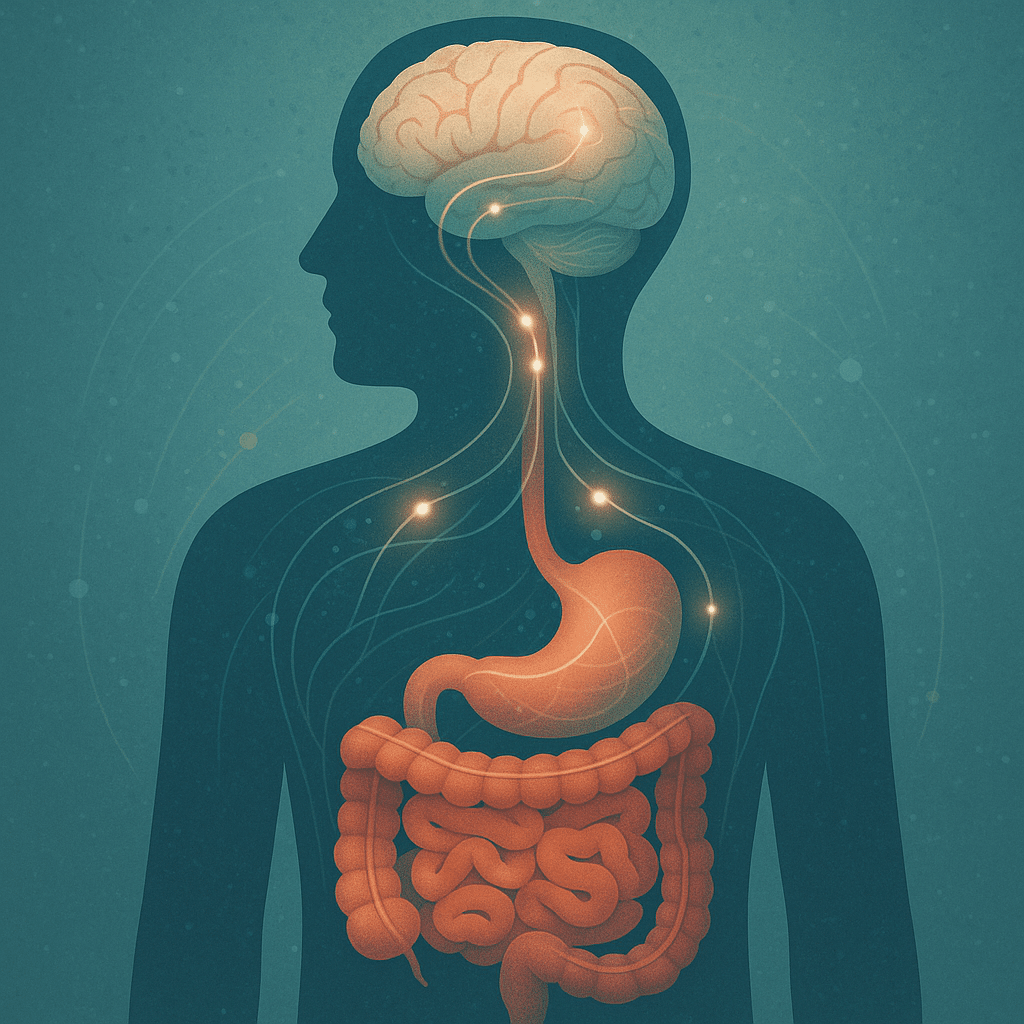
Your digestive system and brain are in constant conversation, sometimes through nerves, sometimes through bacteria, and often through inflammation. When one of them is off, the other notices.
It’s why someone with chronic bloating might also struggle with low mood, or why antidepressants work for some but don’t help others feel quite right. More people are realizing that mental health doesn’t begin and end in the brain. There’s a growing understanding that the gut-brain connection plays a meaningful role in how we feel every day, from our energy levels to how well we handle stress.
Let’s talk about that link, and why your digestive health and mood might be more connected than you’ve been told.
What Is the Gut-Brain Axis?
The gut-brain axis refers to the way your brain and gut talk to each other. This full network involves nerves, hormones, and microbes, the tiny ones living in your belly.
The Vagus Nerve
This nerve is like a two-lane highway connecting your brainstem to your abdomen. It lets your brain know what’s happening in your gut and vice versa. Researchers have found that mood-based improvements from gut therapies often disappear when this nerve gets disrupted. That’s how central it is.
The Microbiome
Your gut houses trillions of bacteria. Some are helpful, while some are not. When that balance is disrupted, your body notices. These microbes influence everything from inflammation levels to the way your body processes nutrients.
A 2025 study found that people with depression had lower baseline levels of butyrate and propionate, two gut-derived compounds. Higher butyrate levels were linked to better remission outcomes, suggesting a potential role in depression recovery.
Chemical Conversations
Tryptophan, an amino acid found in many foods, can go down one of two roads. It can help your body make serotonin, a feel-good brain chemical. Alternatively, if inflammation is high, it might get shunted into a different path, leading to byproducts that can make things worse.
This could explain why some people don’t respond to traditional depression treatment alone.
How the Gut Influences Mood
It’s easy to assume this is just about digestion. But there’s more going on under the surface. Here are three ways the gut can send signals that affect your mood, energy, and ability to manage stress.
Chemical Messengers
When gut bacteria break down fiber, they produce short-chain fatty acids (SCFAs) that help calm inflammation and support the brain. If your body doesn’t have enough, your mood often declines. Research reviewing both people and animal studies found that lower SCFA levels were consistently tied to more intense depressive symptoms, highlighting the gut’s role in emotional health.
Inflammation & Immunity
A leaky gut allows tiny particles to slip into your bloodstream, things your immune system wasn’t supposed to see. This kicks off inflammation, which, over time, can impact how your brain functions.
One study found that people with hard-to-treat depression had clear signs of poor gut barrier health and elevated inflammation.
Stress Loops
When your microbiome is unbalanced, your body tends to overreact to stress. Cortisol spikes, sleep suffers, and your system stays on edge.
That tension isn’t just in your head. It’s in your gut, and it’s creating feedback loops that make everything feel a bit harder.
When Your Gut Might Be Affecting Your Mood
You don’t need to have full-blown digestive issues to be affected. Sometimes, it’s the little signs that stack up.
On the Emotional Side:
- Low-grade anxiety that comes and goes
- Trouble focusing or remembering simple things
- Sleep that feels light, even when you’re exhausted
- Mood swings that don’t track with external stress
Physically:
- Bloating that seems random
- Cravings for sugar or carbs after stressful moments
- Constipation one day, loose stool the next
- Feeling sluggish after meals, even small ones
Why Holistic Psychiatry Sees What Others Miss
It’s easy to feel dismissed when you talk about these symptoms. Many people are told it’s “just stress” or are given a pill without a deeper investigation. Sometimes, that’s enough, but not always.
Holistic psychiatry doesn’t treat your brain as separate from your body. It asks how your digestion, sleep, blood sugar, and nervous system are interacting. It sees your mental health as the result of many moving parts, not just neurotransmitters.
For many patients, that shift in perspective changes everything.
What a More Integrated Plan Might Look Like
No one’s gut and brain look the same. That’s why the process always starts with understanding your personal picture.
The First Step: Look Deeper
A good provider won’t just ask about mood. They’ll ask about your food patterns, bowel movements, energy crashes, and how you sleep. They might run labs, looking at markers like vitamin D, B12, inflammation, or even microbiome composition.
The Plan That Follows
What you’ll get isn’t a one-size-fits-all protocol. It’s a custom plan that might include:
- Shifts in diet: Not a fad diet, but one that supports microbial diversity.
- Gentle routines: Breathwork, morning walks, and stress resets.
- Supplements that serve a purpose: Only what’s needed, not a shelf full of powders.
- Medications (when useful): Integrated with other supports, not relied on alone.
That last one is important. If you’re considering depression treatment, medication can absolutely help. However, it often works better when paired with root-cause support.
Let’s Not Overlook What Your Body’s Been Trying to Say
You’ve probably tried a few things already. Maybe some worked a bit, while others didn’t. If it still feels like something’s missing, that doesn’t mean you’re broken. It might just mean the right questions haven’t been asked yet.
At Zeam, we believe in listening to the whole story. That includes the gut. And that includes how you eat, how you sleep, and how your body reacts to stress. We offer everything from nutritional psychiatry to advanced tools like TMS, neurofeedback, and ketamine treatment, always guided by what works for you.
If you’ve been typing “mental health clinic near me” into search bars, hoping for something that fits, you may have just found it at Zeam Health & Wellness.
If you are in Sacramento, Folsom, or Roseville, contact us. We will help you figure out what’s going on and help you feel like yourself again.
Key Takeaways
- The gut-brain axis links digestion and mood — signals travel through nerves (like the vagus nerve), hormones, and the microbiome, directly influencing mental health. [1]
- Gut microbes play a role in depression — people with depression often have lower baseline levels of butyrate and propionate, short-chain fatty acids (SCFAs) that calm inflammation and support brain function. [2]
- Imbalances in the microbiome affect stress resilience — disrupted gut flora leads to exaggerated cortisol responses, sleep disruption, and difficulty regulating emotions. [3]
- Poor gut barrier health contributes to treatment-resistant depression — inflammation and “leaky gut” markers are elevated in patients who don’t respond to standard therapies. [1]
- Lifestyle and diet can shift outcomes — diverse diets, stress-reducing practices, and targeted supplements can improve gut microbiome balance and mental health. [2][3]
- Holistic psychiatry integrates gut health into care — by assessing diet, sleep, bowel patterns, labs, and inflammation markers, providers build personalized plans that combine therapy, medication, and root-cause strategies. [1][2][3]
References
[1] Zhu Y, et al. Gut microbiota and depression: mechanisms and pathways of the gut-brain axis. Nature Mental Health. 2023
[2] Sciarretta S, et al. Gut-derived metabolites, short-chain fatty acids, and depression outcomes. ScienceDirect. 2025
[3] Pinna M, et al. Gut permeability, microbiome imbalance, and treatment-resistant depression. PubMed. 2023